
The Truth About Frontline Medical Worker PTSD
Donation protected
SUMMARY: Davis is a 53 yo frontline healthcare worker dealing with long covid that is causing ongoing physical health challenges as well as mental health challenges. We need to raise a minimum of $30k ASAP for PTSD services. $54k is the price of treatment.
About Davis the Cardiovascular Perfusionist
About Davis the Cardiovascular Perfusionist
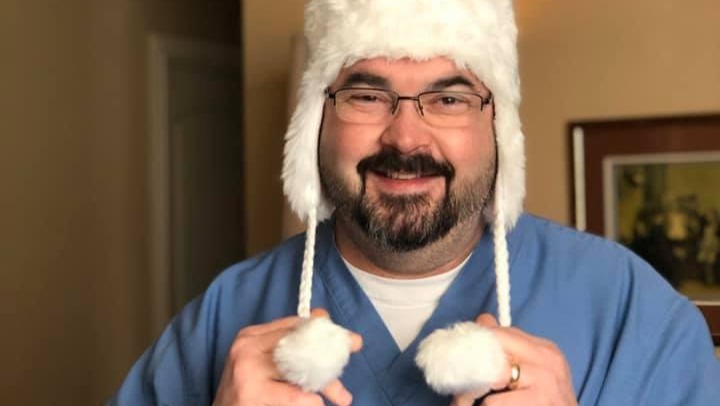
My husband Davis is a frontline medical worker. He’s one of approximately 4000 Cardiovascular Perfusionists in the United States. Davis has over 20 years in the field of perfusion. Prior to that, he was an anesthesia tech at a large hospital in downtown Dallas, TX. You normally see him in the operating room during heart surgery. He's the one who stops your heart and lungs, placing you in animated suspension, and acting as your heart and lungs during open-heart surgery, but perfusionists do so much more. Davis has been a member of heart transplant teams, worked with pediatric heart and craniosynostosis cases, and hyperthermic intraperitoneal perfusion chemotherapy (HIPEC). He sits in on TAVR (valve replacements), VAD (the bridge to help a patient until a replacement heart can be located), and IABPs (balloon pump). He also makes fun things like platelet gels.
Approximately a year before the pandemic, Davis was an integral part of starting the ECMO program at the local hospital. ECMO is a form of life support and is the last-ditch resort to save a person's life, and has played a huge role during the COVID-19 Pandemic.
When Covid first hit this area of Texas and specifically the hospital where he oversaw the perfusion department Davis had to make some decisions most people don’t think about. The first Covid patient needed to be placed on ECMO, who was going to do it? Remember, at that time we didn’t know a whole lot about this virus. All we knew was it was killing people around the world. He looked at his team. One is young and engaged and has a full life ahead of him. One is older than my husband, and my husband who leads the department. The young one shouldn’t go in because he has a lot of life to give that will be needed. The older one was a higher risk profile being closer to retirement. My husband called me, let me know his decision and why, and then suited up and put the first patients on life support. He did this for a while until he felt it was safe enough to let the others do it.
Then July 2021 happened. He got Covid.
Welcome to Delta.
5% of the general population will not fully respond to the covid vaccine. There’s currently no way to tell who that 5% is. This vaccine does not protect you from getting Covid. It does help it not be as bad of a case. My husband Davis was one of that 5% becoming a member of the breakthrough covid cases. Delta moves MUCH faster and MUCH harder than previous variants. He did end up in the hospital. He was treated with Remdesivir. The vaccine worked in that had this been July 2020, he would have died. I know this in my soul.
When he was released from the hospital, he was technically cleared of Covid, however, Covid wasn’t done with him. Davis continued to worsen. We learned this is not uncommon. He couldn’t walk ten feet without his O2 sats dropping below what the pulse oximeter measures. He was placed on home oxygen, nebulizer treatments, inhalers, more steroids, and antibiotics. This treatment continued for approximately a month when he began having more issues.
As he began not being able to breathe and coughing the strangest cough I’ve ever heard and begun turning blue, we went back to the hospital. Three PEs and a DVT. All were too small to treat interventionally, the decision was to administer lots of heparin. Turns out his body ignores heparin. He was put on a different blood thinner, and continues on it and likely will for the rest of his life.
Once Davis was stabilized, he was released again and returned home. He continued being on oxygen. He was still weak, and he was unable to work. It was at this time he was informed it was possible he may never go back to work. Oh, and now he has a heart issue, and PTSD from being a frontline healthcare worker watching people die and as a patient thinking he was going to die. PTSD, depression, and anxiety. Trifecta. Davis is a helper. You know the ones “in times of trouble look for the helpers.” That’s my husband. But he can no longer help. He can’t do what he was put here to do. Or that’s what he believes despite what I and others may say to him. As some of you may or may not understand, not being able to help, do, provide, etc., is the worst thing that can happen to Davis.
Men in their 50s are one of the highest risk for suicide. Suicide among healthcare workers and doctors is increasing exponentially due to the pandemic. Sunday, September 26, 2021, started out like most days. We were making plans for the future. All seemed relatively well, but as the day went on, his day became more difficult. We have bad days - combo of health, capabilities, and mental health toll on not being able to do all the things. However, his normal bad day took a sudden turn. Long story short, he attempted and almost succeeded in suicide. One ambulance ride later, Davis was placed on a ventilator. His CT didn’t show any brain bleeds so he was back on blood thinners. We didn't need additional PEs or DVTs. He began responding. He only responded to three things: my voice, music (played him one song), and pain. When he would hear my voice he would wake up some and start fighting which would cause coughing which caused pain. By the following morning, he was moving all extremities, was able to lift his head, and tried to talk. We began communicating via hand squeezes. He knew where he was. He knew why. He let me know he was in pain - throat, and lungs. He didn’t know he was on a vent. Once I explained that he relaxed some. His nurse upped his sedation to let him rest since we knew he was ok.
Healthcare workers are not doing ok. They may look ok. They come to work and they do their jobs, but they are NOT OK. I told his nurse I was happy to see the ER wasn’t overflowing. He looked at me and said, “it’s a lull. But you’re right. It’s better. We’re down to 100% capacity here in the ICU. We’ve been at 120-130% for so long that 100% feels like a vacation, but we’re still drowning.”
“When workers get sick, they may feel helpless or guilty about being unable to perform their essential, life-saving jobs, or for contributing to staff shortages for those remaining at work. The late Dr. John Mack, a noted suicide expert, wrote, “low self-esteem results when a wide gulf is experienced between the perceived self and the ideal self.” Suicide can result when individuals judge that they do not measure up to their “ego ideal,” the person they wish to be. Health care workers are often motivated by wanting to help others. Being rendered helpless in the midst of the COVID-19 pandemic may affect their self-esteem and identity, increasing suicide risk.” Citation
There was zero judgment from the staff at the hospital. They all understood. They know these feelings all too well. They aren’t heroes anymore. They were early on. They aren’t now. People take care of their heroes. Our healthcare workers are fighting often alone and struggling physically, emotionally, and mentally.
There is no shame in breaking.
My husband was on a ventilator because he’s a helper. He’s a helper who can’t help. Remember, when things go bad look for the helpers? We were very blessed Davis was able to be off the vent in just under 24 hours. Between the tons of charcoal and other interventions, he was spared quite a bit. He is now home. It has been determined he has extreme PTSD. The issue we have now is the treatment he so desperately needs costs $54,000. It's a 45-60 day inpatient facility that specializes in medical professionals just like him. Davis has offered to sell his truck to pay for half. If we can raise half the funds, we will sell the truck and get him there. Insurance does not cover this. They'll cover a couple of weeks of inpatient in a drug and alcohol facility, but that's not his issue. The counselor we spoke with said he hadn't seen a case of PTSD this bad since working with Viet Nam vets. As Davis's wife, I didn't know how I felt about that - relief or ... but I finally felt someone was listening. The medical staff will work with Davis on mental health and physical health healing.
Davis didn't and doesn't want to die. That was never his first choice. He needs peace. He needs the nightmares to end. He needs support. He needs to be heard and treatment that isn't a pile of pills to try to numb his current and past year and a half reality. This is what we are asking for. Cardiovascular Perfusion is my husband's passion. He would like to be able to go back to work. If he can't go back to work due to dependency on oxygen, ok, but I can't in good faith look my husband in the eye and say I tried everything to help if I don't try this. I put we need $54k. If we can get to $30k, again, Davis will sell his truck for close to $28-28k. This was his own suggestion. We can replace a car. We can't replace Davis. We've gone through all of our savings. We will be able to pay bills when he receives long-term disability beginning in November when the first payment rolls out. I expect to be working full-time again by late October. My offer letter should be here in the next couple of days. We aren't asking for help for anything other than this treatment. They require payment upfront. Insurance does not cover this. His therapist recommended this program. We checked it and another one out. If there are any funds left, we will donate them to other healthcare workers going through the same things. If someone wants to help me set up a non-profit for this specific purpose, please let me know.
Thank you for reading our story. If it speaks to you at all, please share. It's more important to us that this story is told. Yes, he needs treatment, but if that can't happen, maybe his story will somehow help others struggling with the same things.






Organizer
Lisa Hunt
Organizer
Sherman, TX