This isn’t just my story—it’s proof of how systemic barriers warp justice. What happened to me could happen to anyone. That’s why I’m speaking out… and fighting back.
––––––––––
SHORT VERSION
I went in for a routine knee arthroscopy in February 2023. When I woke up, I had a long incision—something I did not expect and had never been discussed with me beforehand.
When I tried to understand what happened, I couldn’t get clear answers, and the sharp, radiating pain I was experiencing went unexplained. A second surgeon later found severe bone and cartilage damage in an area that had been normal on my pre-op MRI. During a follow-up surgery, a metal fragment was discovered inside my knee, along with permanent bone loss where a fracture had occurred.
I pursued legal action because I needed answers. Instead, after presenting my evidence, I was offered a settlement—on the condition that I sign an NDA and stay silent.
I refused.
That decision preserved my voice, but it came at a massive cost. My attorney later withdrew, not because of a lack of evidence, but because Texas law makes cases like mine financially impossible to take to trial. Doctors aren’t required to carry meaningful malpractice insurance, and damage caps severely limit accountability. In my case, the surgeon carried just $200,000 in coverage, far below my total damages.
Soon after, the defense moved to dismiss my case, claiming there was no evidence.
No evidence, they argued, that an unnecessary incision had been made.
No reference to the metal fragment later found inside my knee or to the surgeon’s sworn deposition testimony explaining the incision.
The court adopted their Sept. 2 proposed order verbatim without addressing my pending filings from late Sept. or early Oct. My case was procedurally shut down, without the court ever grappling with the evidence or sworn testimony already in the record.
Put plainly: refusing the NDA preserved my voice, but the system responded by making justice inaccessible. This campaign exists because silence should not be the price of justice.
I’m crowdfunding to keep this case alive—not just for myself, but to expose a system that quietly pushes harmed individuals into gag orders instead of truth and accountability. The initial goal of $25,000 is to retain an appellate attorney to pursue the appeal—the step required to get the facts of what happened actually heard by the court.
The deadline to preserve my appeal rights is January 8, which means the window to act is narrow and closing fast.
If the case is returned to trial court, remaining funds will go toward the resource-intensive trial stage expenses and to secure a trial attorney. Any funds beyond that will be directed toward patient-safety advocacy, including efforts to challenge the use of NDAs that silence individuals and keep harm out of public view.
This is what David versus Goliath looks like in modern healthcare.
I refused to be silenced. Now I’m fighting to be heard.

One month before the injury. I was active, adventurous, and living without limitations I have today. I’m fighting to reclaim the version of myself this photo represents, which is why it's my lead.
––––––––––
LONG VERSION
Full story and background below for anyone who wants to understand the bigger picture.
Disclaimer: This campaign is not a decision I made lightly. After my lawyer withdrew due to systemic economic barriers—and after dozens of other attorneys told me that my case, despite its merits, is not economically viable under Texas’s restrictive laws—I chose a creative, transparent, and yes, terrifying path as the only avenue left. This campaign is about a system that too often leaves harmed patients unheard and unprotected—boxed out from justice by inadequate insurance, unjust damage caps, insurer loopholes, procedural tactics, Texas efficiency culture, financial liens, and gag clauses (NDAs).
The sad truth is: stories like mine play out every day, quietly and painfully. Texas may be ground zero—but fault lines exist nationwide.
I always knew I wanted to one day draw on my experience to drive reform. It’s the reason I turned down the comfort of a quick resolution that would have stripped my voice, even at great personal cost. It’s also why I’m speaking out now, despite the risks—and putting on my advocacy hat earlier and louder than I ever planned.
At the end of the day, I want what happened to me to matter and to drive positive change. My aim is a safer, fairer system so no one else endures what I have.
Note: Everything I share here reflects either my lived experience or facts from the public record. This campaign is NOT about proving my case—that belongs in the courtroom. It’s about using my story to highlight the laws and practices that keep patients from fair access to justice and undermine transparency in healthcare. I’m asking for a chance to access a system that’s supposed to protect everyone equally, whether institution or individual.
––––––––––
THE SURGERY THAT CHANGED EVERYTHING

February 2023—the incision I woke up to. This was not the arthroscopic procedure I consented to.
To understand why I’m fighting, you have to know what happened.
In February 2023, I walked into the operating room for what should have been a routine knee arthroscopy.
I woke up with a lengthy incision I hadn’t consented to—and an operative report that omitted the incision, characterized the procedure as an arthroscopy, and recorded the tourniquet time at 47 minutes. By contrast, the OR nursing notes documented 72 minutes.

Severe bruising directly after the February 2023 procedure
After suffering weeks of unexplained radiating pain, I sought the help of another surgeon, who discovered severe cartilage damage on the outside of my knee—a large grade 4 lesion with exposed bone. I was told the underlying bone had been fractured, resulting in permanent bone loss.
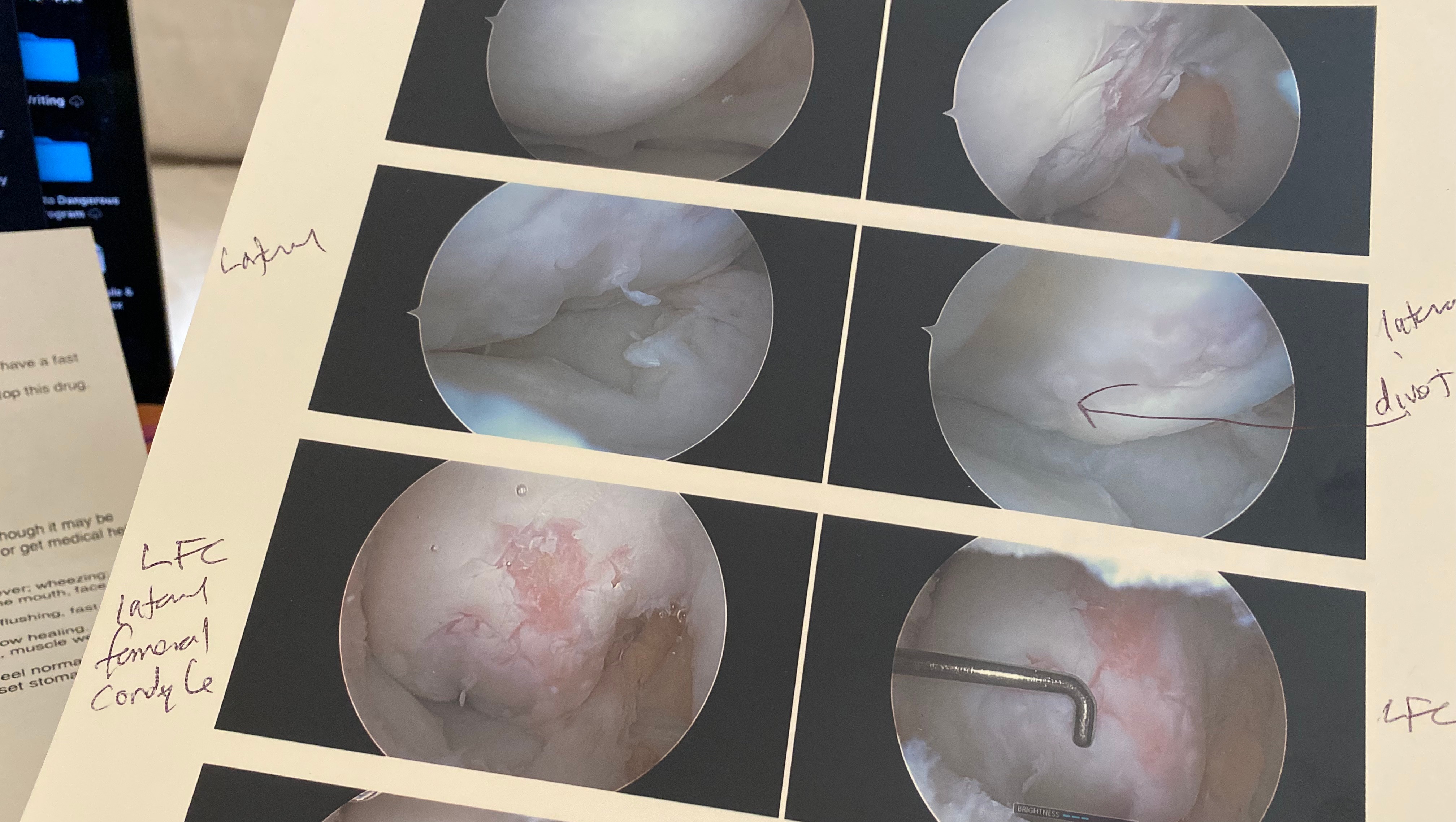
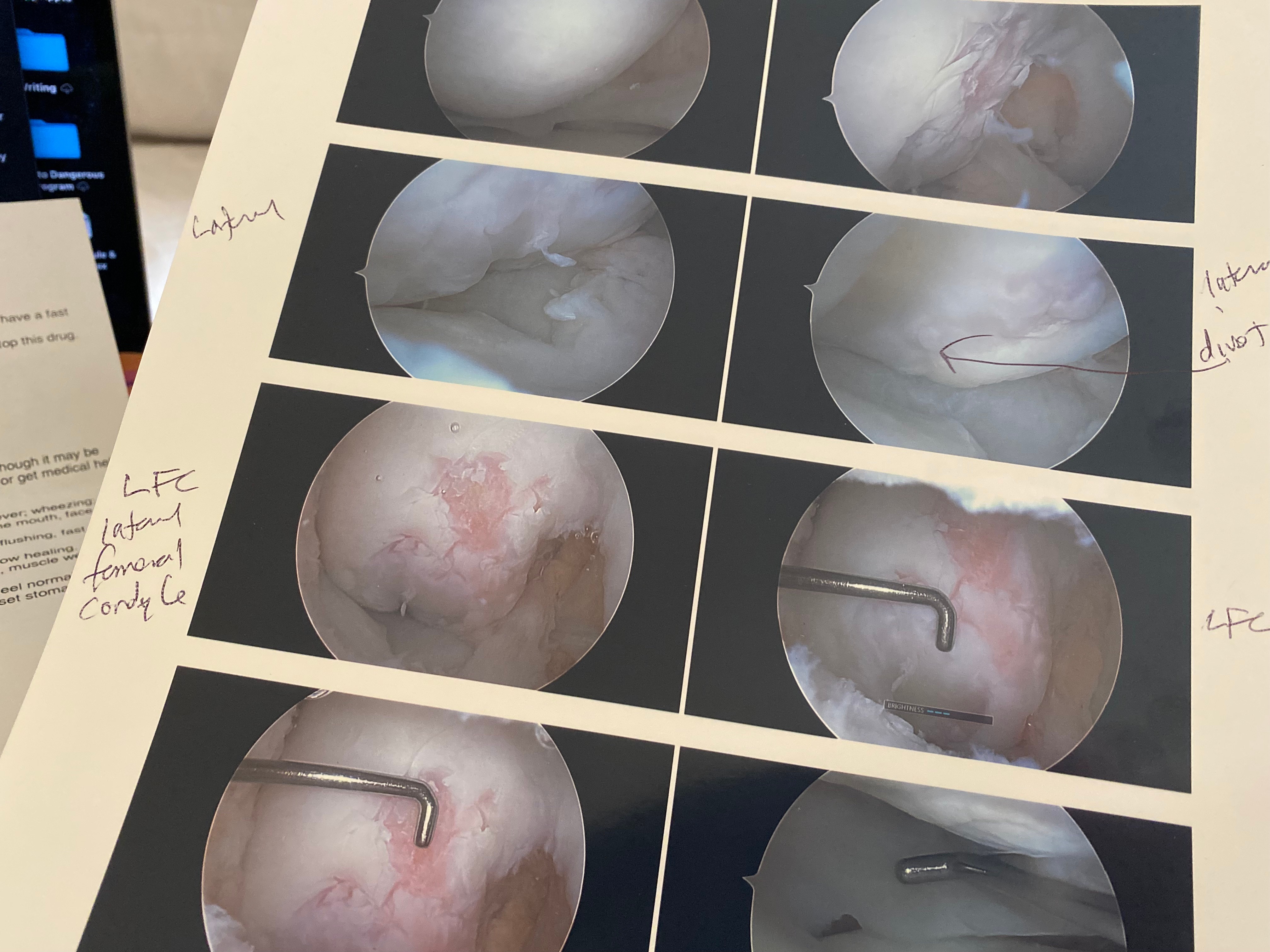
Images from the second surgeon’s investigative arthroscopy showing the severe cartilage damage and divot in the bone where the fracture occurred.
In a subsequent investigative arthroscopy, the second surgeon found a metal fragment inside my knee.

The metal fragment discovered inside my knee during the second surgery.
My life changed overnight. Since that Feb 2023 procedure, I’ve endured multiple subsequent surgeries, chronic pain, lost wages, PTSD, and the loss of the active lifestyle that once defined me—running, aerial ropes courses, dancing, volleyball, even surfing.

Before the injury, I was active and athletic. I had no activity limitations as a result of my knee.
For me, the not-knowing has been as devastating as the injury itself. I may never have a clear answer about what exactly happened to me while I was under anesthesia.
Yet when it came time to resolve the case, there was a catch.
My silence.
The offer to resolve was contingent on confidentiality.
I refused. To lose my voice felt like another injury, not justice.
––––––––––
THE PRICE OF SILENCE
But here’s the problem with my decision: refusing silence meant risking my own case. In Texas, medical malpractice cases are nearly impossible to take to trial.
Here’s why:
- Trials are expensive. It often costs $80–150k+ just to reach a jury. Attorneys usually front those costs and only get paid if they win, taking about 40% in contingency fees.
- There’s a cap on damages. No matter the suffering, Texas law limits what an injured patient can recover for pain, suffering, or loss of quality of life to $250k—unchanged since 2003. These caps disproportionately hurt vulnerable groups without high economic damages (seniors, children, stay-at-home parents, disabled patients, low-income workers), leaving them with little to no recourse despite catastrophic harm.
- This cap also incentivizes some physicians to carry minimal insurance, sometimes less than the $250k cap itself. There is no malpractice insurance mandate in Texas.
Layer on Texas debtor-protection laws—which make it nearly impossible to collect beyond insurance—and the risk of drawn-out appeals, and it’s clear why attorneys can’t justify fronting cases like mine, even when they truly wish they could help.
Illustrative Example:
• Insurance policy limit: $200,000
• Attorney contingency fee (40%): $80,000 → $120,000 remaining
• Trial and expert costs (often fronted by the firm): $80,000-$100,000 → $20,000–$40,000 left
• Medical liens: $20,000+ → Net recovery for the patient: $0–$20,000
This is how the system ensures these cases rarely see daylight. Harmed patients are left feeling forced to accept settlements conditioned on NDAs—and future patients never find out.
Instead of becoming another silenced statistic, I decided to call it out.
The result? In August 2025, my attorney withdrew. Since then, 40+ attorneys have told me some version of: “Valid case, but not economically viable.”
This happens every day. And Texas isn’t alone. Many states across the U.S. have laws in place that protect institutions at the expense of transparency and patient safety.
Patients like me are forced to drop their cases—or, if they’re “lucky,” to choose between their case and their right to speak openly. Harm goes left unchecked. Silence wins.
But silence only convinces lawmakers that the system’s working. And complacency keeps that illusion alive. The cycle continues.
––––––––––
PATIENT VS SYSTEM
In many ways, this case has become a personal mission for me.
It’s now patient vs. system.
The Defense quickly turned to procedural maneuvers once I was in a position of vulnerability without counsel. They filed a motion asking the judge to dismiss my case, claiming I have ‘no proof.’
I had to learn how to draft and file my own pro se response and research the relevant case law to cite. That motion was the turning point. It was the moment the system—Goliath—proved my point and clarified why I had to fight.
It was also the moment Goliath accidentally handed David a slingshot. And a few rocks.
Still, without counsel, the system is designed to crush me. The court dismissed my case without explanation—without addressing my response or evidence, without ruling on my motion to extend the hearing date, and without giving me the opportunity to appear.
The judge signed the Defense’s order verbatim.
My pending pro se filings went ignored, raising serious questions about whether the system values efficiency over justice—and reinforcing my point:
The system is designed to protect itself. It muzzles people like me before they can be heard.
But I won’t make it easy. I recently filed a Motion for New Trial to assert my right to due process. Should that go ignored, I’m prepared to take it to the appellate court—with a January 8 deadline to preserve my appeal rights.
That clock is already ticking. It’s why every day and every share matters now. This fight isn’t just about one ruling.
That’s why I’m here. Despite being a very private person—and this being the most terrifying thing I’ve ever done—I believe in speaking up when it matters.
For journalists, attorneys, and advocates (optional reference):
For those who want to review the procedural issues being appealed, a redacted copy of my Motion for New Trial (a public court filing) is available here. This document is shared for transparency and context, not as a substitute for the court process.
––––––––––
WHY THIS FIGHT MATTERS
We all depend on medical care. Most of the time, our healthcare providers are true heroes. My current health team has been my strongest support in this battle.
But physicians are human, and mistakes happen. When they do, the justice system should be there to protect us, not bury the harm.
The real path to fewer lawsuits isn’t damage caps. It’s transparency. When physicians and hospitals are incentivized to disclose errors honestly and handle them ethically, both patients and providers are protected—and lawsuits become rarer (see: University of Michigan Health System).
Doctors and nurses deserve a system where honesty safeguards them as much as it safeguards patients.
Lawsuits are grueling—physically, emotionally, and financially. No patient already suffering chooses this path unless there’s no other choice.
I’m not doing this for money.
Even if I ‘won,’ the economic limits tied to my case would cover only a fraction of my actual losses. I’m doing this for justice, and in hopes that speaking out—however reluctantly—will expose the human cost of these barriers and move the needle toward real change.
The fact that I have to crowdfund just for a chance of getting in front of a jury proves how broken the system is.
Your support will help ensure my case is decided on its merits—rather than buried by a procedural dismissal. Most importantly, it will force the system to confront itself.
––––––––––
WHY YOUR SUPPORT MATTERS
Your support will:
1. Give me a fighting chance to retain new counsel and bring my case before a jury
2. If that proves impossible, fuel broader advocacy for patient safety and reform
3. Send a powerful message that the justice system should protect all of us
If you can’t donate, you can still help:
• Share this campaign.
• Call your lawmakers. Demand mandatory meaningful insurance, an end to damage caps, and a ban on NDAs. NDAs silence victims, hide patterns of negligence, and block systemic accountability and learning. Over time, they’ve evolved into a tool of control, shielding power and muting truth. First Amendment rights should not be for sale. Transparency makes the system safer for everyone.
Every dollar, every share, every voice matters. I refused to be silenced. With your help, I can finally be heard.
Special thanks to the attorneys and legal professionals who generously reviewed my campaign pro bono to ensure clarity, fairness, and First Amendment compliance.
Important note regarding press inquiries:
Because my case is ongoing, I cannot comment on the specifics of the underlying alleged harm. However, I can speak to my experience navigating the system, my values around transparency, and the broader issues that affect patients everywhere.
–––––––––––––––––––––––––––––––––––––––––––––––––––-
Funding & Transparency Statement
Donors understand that contributions are voluntary donations, not investments, and they create no expectation of financial return or influence over legal decisions.
All funds raised through this campaign will be managed responsibly in a segregated account and used exclusively for legal expenses related to my case, including appellate filings if needed, expert witness fees, deposition transcripts, court filings, exhibits, and trial preparation costs. Funds may also go toward addressing other barriers such as a fee lien asserted by prior counsel after withdrawal and an unaddressed health insurer lien under my employer-sponsored plan.
Any funds raised beyond baseline trial expenses will support next legal steps if needed and/or longer-term advocacy efforts.
This campaign is not a guarantee that I will secure new counsel or get my chance at justice. Nothing is ever guaranteed in a capped system tilted against patients. But your support allows me to overcome one major barrier to justice that is within my control.
If circumstances change, I will provide transparent updates about how funds are used. Whatever the outcome, funds will stay directed toward advocacy efforts.
All views and initiatives expressed on and off this platform are my own and reflect my personal advocacy as a private citizen. They are not affiliated with or endorsed by my employer.
All filings are public via the Harris County District Clerk’s site (Case No. 2024-26072).
---
Want to Learn More?
Why does this system reliably end in silence, NDAs, and procedural dismissals? If you’re curious, here’s the legal architecture that makes outcomes like these inevitable, along with resources I found helpful during my own research:
· Texas Tort Reform: How 2003 laws capped non-economic damages and made malpractice cases economically impossible for patients to pursue. These caps disproportionately affect vulnerable groups who don’t have high economic damages (i.e., low-income workers, unemployed individuals, children, disabled patients, homemakers), leaving them with little to no recourse despite catastrophic harm. → Law Review 2003 Caps | Economic Study Tort Reform Fallout | American Progress Accountability Lost
· Other States: See which states have similar tort reform laws and which have already ruled such restrictions unconstitutional. → Comparative Map of Caps & Challenges
· Lack of Transparency and NDAs: Research shows that malpractice litigation has long been shaped by a “deny and defend” culture, where errors are hidden, patients are silenced with NDAs, and systemic learning is blocked. → Georgetown Law NDAs & Malpractice Harm | PubMed Gag Clauses in Healthcare | NBC News Silencing Patients | Health Journalism NDAs & Unsafe Care
· Transparency as a Path to Fewer Lawsuits: Studies of disclosure-and-resolution programs show that when hospitals commit to full transparency—acknowledging errors, apologizing, and compensating patients fairly—lawsuits become rarer, cases resolve faster, and costs fall for both patients and providers. → AAMC Best Response to Medical Errors Is Transparen | Understanding Barriers to Error Disclosure | The CANDOR Model - The Gold Standard for Honesty | CMS - A National Accountability Framework
· The Stowers Doctrine: Why insurers have a duty to settle reasonable settlement demands within policy limits. → Versus Texas Stowers Explained
· Consent-to-Settle Clauses: These clauses were demanded by physicians, but they have consequences. → Consent Clauses Trap Patients
· Texas Courts on Stowers: Texas courts have ruled that insurers can’t contract around their Stowers duty—so why are “consent-to-settle” clauses allowed to undermine it in medical malpractice policies? In practice, these clauses allow insurers to shield themselves behind a physician’s refusal to settle, even when that refusal is driven by unreasonable non-economic conditions the Stowers Doctrine does not permit, such as prioritizing reputational protection through an NDA. → Court rulings vs Insurer Loopholes
· No Insurance Mandate: Unlike car drivers, Texas doctors aren’t required to carry malpractice insurance. The absence of a statewide minimum coverage requirement, combined with Texas’s low non-economic damages caps, incentivizes some physicians to carry minimal coverage, leaving patients exposed when serious harm occurs. → DrsCoverage No Mandate in Texas
· Debt Protection State: Texas shields professionals with debtor protections, making it very difficult to collect judgments even if you win. → Texas Shields from Judgments
· Pro Se Litigants and Structural Disadvantage: Civil courts emphasize neutrality, but the system is built around counsel-driven litigation. Empirical research consistently shows that pro se litigants face lower success rates and reduced judicial engagement with filings, particularly in procedurally complex cases. This disparity is structural and it becomes most pronounced once counsel withdraws. → Pro Se Litigants and Outcome Disparities | How Pro Se Status Shapes Judicial Decision-Making
· Summary Judgment as an Efficiency Gatekeeper: In theory, summary judgment is meant to dispose of cases lacking genuine factual disputes. In practice, Texas’s "no-evidence" summary judgment (MSJ) culture in medical malpractice cases is heavily driven by a statewide emphasis on judicial efficiency. New legislation (SB 293 and HB 16, effective September 1, 2025) formalized efficiency and docket management as factors in judicial performance evaluation. Although the legal standard requires only a “scintilla” of evidence (anything more than mere suspicion) to survive a no-evidence MSJ, this efficiency-driven environment—reinforced by recent Texas Supreme Court rulings and persistent docket pressure—can incentivize judges toward dismissal. Notably, defense firms may argue that a plaintiff has “no evidence” at summary judgment even after previously seeking to settle and offering payment because of that same evidence. → Questionable Summary Judgments in Texas Courts | SB 293 Judicial Efficiency & Summary Judgment Proc
· Subrogation Liens as Hidden Barriers: Even when a malpractice claim has strong evidence, subrogation liens can shift financial risk back onto injured patients, discourage attorney involvement, and reinforce pressure to resolve disputes quietly and early. → Subrogation Impact on Recovery in Capped Cases