Kinsley's Surgeries
Donation protected
Nick and I became pregnant and found out that we would be welcoming a baby girl midsummer. An abundance of excitement led to the creation of a beautiful nursery and an incredible baby shower. All was well.
Four weeks before our due date we went in for our final ultrasound. My OB doctor entered the room and sat down. He folded his hands quietly and after a moment of silence he laughed halfheartedly and said, "your ultrasound has shown us some surprising results."He explained that our pregnancy was what is called an "SAU pregnancy" or "Single Umbilical Artery", meaning that our baby's umbilical cord was a two vessel cord made up of one vein and one artery rather than the normal three vessel cord with one vein and two arteries.
The doctor explained that this is something typically found during the anatomy scan at twenty weeks, but it appeared that our scan at that time showed a normal cord, so one of the arteries must have stopped growing altogether or fused in with the other artery-- they weren't really sure.
There was a lot they weren't sure about. He told us that when a single umbilical artery is found, sometimes the baby will be born with other congenital and/or chromosomal defects, but since our ultrasounds were all normal, he assured us he was confident we wouldn't face any of these defects.
I spent the next three weeks trying to emotionally and mentally prepare myself for the worst, hoping, praying, and expecting fully that it would not come to that. I was wrong.
We had a natural, vaginal, drug free birth, and after six hours of active labor and 26 minutes of pushing, our daughter, Kinsley June, was born Sunday, June 25th, at 7:37pm; a modest 6lbs, 11ounces, and 19.5 inches long. She was placed on my chest, the doctor began stitching me up, and not five minutes later she was taken from me, placed on a table under a beaming light where four nurses hovered over her limp, blue body, trying to suction her throat, count out loud and with two fingers pump air into her lungs simultaneously. After minutes that felt longer than my life, they were successful and she began to breathe again. Temporarily.
I did not hold my daughter again for eight days, as she was taken to the Helen DeVos Children's hospital for surgery in Grand Rapids, Michigan, which is over 200 miles and 3 hours from our home. I was given a cloth scent doll that I held all night in place of my newborn baby who was taken from me. The following morning I was discharged from the hospital in Petoskey, and after going home to grab a few things, we drove to Grand Rapids where we've been ever since. We have spent almost four weeks at DeVos now.


As it turns out, Kinsley was born with three congenital defects: Tracheoesophageal fistula (TEF), Esophageal Atresia (EA) and an Anterior Anus.
TEF and EA are responsible for her stopping breathing a few minutes after she was born. TEF is an abnormal connection between the upper part of the esophagus (tube that carries food from mouth to stomach) and the trachea or windpipe (tube that carries air into and out of lungs), and is a condition that affects 1 in 4,000 children. It often occurs with EA, which is when the upper part of the esophagus does not connect with the lower esophagus and stomach. Both defects are life threatening and must be corrected by a pediatric surgeon immediately following birth.
Basically, the throat opens to two tubes, the trachea which branches off into the lungs, and the esophagus which takes food to the stomach. From the mouth, Kinsley's esophagus began but dead-ended in a small pit. The bottom part of her esophagus which should have connected at that pit was instead connected to her trachea. This means that stomach acid and other fluids from her stomach could go into her lungs, and anything that she did swallow would go into the pit and then come back up and go down her trachea instead, causing her to choke and stop breathing.
Surgery to correct this involves going in through the side between two ribs to first disconnect the lower esophagus from the trachea and then open up the upper esophagus pit and then attach the two pieces together.
36 hours after Kinsley was born this surgery was performed. After five hours, the surgeon came out and told us it was successful. He was able to rewire her insides and predicted a 3-4 week recovery.


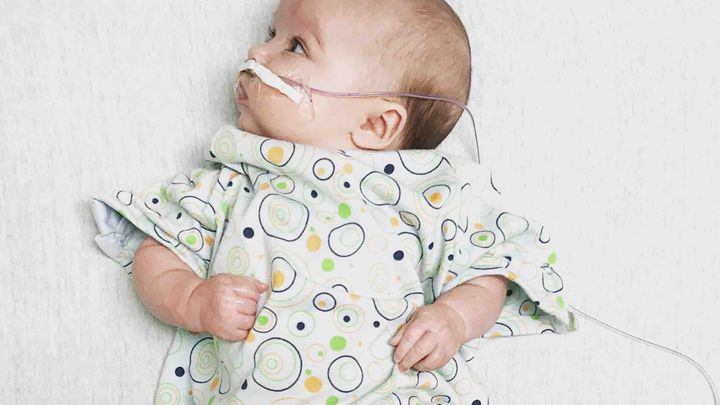
Kinsley came out of surgery with a chest tube to drain fluid and blood from her lungs, an IV in her arm to deliver TPN and lipids, and a feeding tube in her nose since she would be unable to feed for the time being. On the 3rd of July her chest tube came out and we were able to hold her for the first time. A few days later they replaced the IV in her arm with a picc line in her head, which is a more permanent IV that doesn't need replacing as often. For a brief time she was on CPAP, just to open her airway and help her breathe while recovering. Soon after, a video swallow test was done to make sure there were no holes in her esophagus and to verify that everything was healing well and no narrowing was occurring. The surgeon reported that the results were promising and we would be able to start feeding her.
In addition to a full recovery, in order for Kinsley to come home the doctors needed to see that she was gaining weight and taking full feedings every three hours by mouth without needing to use the feeding tube in her nose.
She started out strong, taking half of her feedings by mouth with the bottle, and latching at the breast like a champ. Often she would become exhausted halfway through feeding and fall asleep, so the remainder of her bottle (60-70%) was put in her feeding tube. Every time we fed her she tolerated the full feeding without spitting up. This went on for a few days until she stopped eating and was unconsolable. The doctors determined that she had acid reflux and started to give her Zantac to combat it. From there we had more success with feeding, all the way to the point that she was taking 50% on her own. At 80% the feeding tube can come out, and we were hopeful that we would get there soon.

Unfortunately, Kinsley began having episodes where she stopped breathing during feedings. Two times medical attention was required to bring her oxygen back up to safe levels. At that point, the neonatologist ordered that she been seen by the Occupational Therapist (OT), who came to watch her eat. On the 17th feeding by mouth was deemed unsafe due to oxygen desaturation and her color turning as a result.
OT ceased oral feedings and decided it best to have the Ears/Nose/Throat (ENT) doctor see her and order a new course of action. That evening ENT took a look at her throat and reported that her strider was one of the worst they'd ever heard, and there most definitely was extra floppy tissue blocking her airway.
Currently, ENT has ordered a 48 hour cease on her oral feedings to see if the swelling in her throat will go down so that they can do a bronchoscopy. Depending on the results of that test, ENT will determine with the pediatric surgeons whether or not the extra tissue will have to be surgically removed. It has been said that this is the most likely outcome. So, to recap, this is where we're at:
June 25- Kinsley is born
June 27- Surgery
June 29- CPAP
June 30- IVs out, Picc line in
July 2- Morphine stopped, CPAP off
July 3- Swallow Test, feeding began
July 6- Acid Reflux discovered, Zantac started
July 10- Taking 35% of feedings
July 14- Taking 50% of feedings
July 15/16- Stopped breathing
July 17- OT stopped oral feedings, ENT ordered Bronchoscopy
July 18- Surgery is being discussed
A second surgery means starting back at square one, where we began three weeks ago. Our daughter will be put under again, she will have a breathing tube and feeding tube, IVs will be replaced and a picc line will be put back in her head. We will be unable to hold her, unable to dress her, and she will have to learn to eat all over again after she recovers from this second surgery. All of the progress she has made will be erased.
The emotional burden is immense; maybe you know what it is like to live out of your backpack, miles from home- maybe you can remember a time where it took all your strength to get to the next minute of every day- it's possible that a stressful situation has robbed you of your appetite and sense of calm, among other things- and perhaps you can imagine what it is like to jump at the sound of your cell phone because every call could be the news that causes your undoing. It has been a long three weeks of this, and our journey is only just beginning.
These are all things Nick and I have been overcoming together. However, after three weeks off work, Nick has had to return to Petoskey to pay the bills, as our financial resources have been stretched to their limits. Now that he has had to return to work, we have to overcome these emotional struggles 200 miles apart, and on our own.
It has been a long three and a half weeks. We have recognized our need for help, and we feel it is now time to ask for it.
It is my hope that in sharing our story, by the kindness of people's hearts, the stresses of the financial burden can be lessened. Any donations made will help cover Kinsley's medical expenses not covered by insurance and the living costs such as food and a room for our extended stay at the hospital.
From the bottom of our hearts, we thank you for taking the time to read our story. We thank you for your positive thoughts, vibes, and prayers. If you are unable to contribute to the fund, please share our story with people you know, and continue to keep our sweet baby in your thoughts and prayers- she needs them now more than ever. We will get through this...she is refusing to sink.

Four weeks before our due date we went in for our final ultrasound. My OB doctor entered the room and sat down. He folded his hands quietly and after a moment of silence he laughed halfheartedly and said, "your ultrasound has shown us some surprising results."He explained that our pregnancy was what is called an "SAU pregnancy" or "Single Umbilical Artery", meaning that our baby's umbilical cord was a two vessel cord made up of one vein and one artery rather than the normal three vessel cord with one vein and two arteries.
The doctor explained that this is something typically found during the anatomy scan at twenty weeks, but it appeared that our scan at that time showed a normal cord, so one of the arteries must have stopped growing altogether or fused in with the other artery-- they weren't really sure.
There was a lot they weren't sure about. He told us that when a single umbilical artery is found, sometimes the baby will be born with other congenital and/or chromosomal defects, but since our ultrasounds were all normal, he assured us he was confident we wouldn't face any of these defects.
I spent the next three weeks trying to emotionally and mentally prepare myself for the worst, hoping, praying, and expecting fully that it would not come to that. I was wrong.
We had a natural, vaginal, drug free birth, and after six hours of active labor and 26 minutes of pushing, our daughter, Kinsley June, was born Sunday, June 25th, at 7:37pm; a modest 6lbs, 11ounces, and 19.5 inches long. She was placed on my chest, the doctor began stitching me up, and not five minutes later she was taken from me, placed on a table under a beaming light where four nurses hovered over her limp, blue body, trying to suction her throat, count out loud and with two fingers pump air into her lungs simultaneously. After minutes that felt longer than my life, they were successful and she began to breathe again. Temporarily.
I did not hold my daughter again for eight days, as she was taken to the Helen DeVos Children's hospital for surgery in Grand Rapids, Michigan, which is over 200 miles and 3 hours from our home. I was given a cloth scent doll that I held all night in place of my newborn baby who was taken from me. The following morning I was discharged from the hospital in Petoskey, and after going home to grab a few things, we drove to Grand Rapids where we've been ever since. We have spent almost four weeks at DeVos now.


As it turns out, Kinsley was born with three congenital defects: Tracheoesophageal fistula (TEF), Esophageal Atresia (EA) and an Anterior Anus.
TEF and EA are responsible for her stopping breathing a few minutes after she was born. TEF is an abnormal connection between the upper part of the esophagus (tube that carries food from mouth to stomach) and the trachea or windpipe (tube that carries air into and out of lungs), and is a condition that affects 1 in 4,000 children. It often occurs with EA, which is when the upper part of the esophagus does not connect with the lower esophagus and stomach. Both defects are life threatening and must be corrected by a pediatric surgeon immediately following birth.
Basically, the throat opens to two tubes, the trachea which branches off into the lungs, and the esophagus which takes food to the stomach. From the mouth, Kinsley's esophagus began but dead-ended in a small pit. The bottom part of her esophagus which should have connected at that pit was instead connected to her trachea. This means that stomach acid and other fluids from her stomach could go into her lungs, and anything that she did swallow would go into the pit and then come back up and go down her trachea instead, causing her to choke and stop breathing.
Surgery to correct this involves going in through the side between two ribs to first disconnect the lower esophagus from the trachea and then open up the upper esophagus pit and then attach the two pieces together.
36 hours after Kinsley was born this surgery was performed. After five hours, the surgeon came out and told us it was successful. He was able to rewire her insides and predicted a 3-4 week recovery.


Kinsley came out of surgery with a chest tube to drain fluid and blood from her lungs, an IV in her arm to deliver TPN and lipids, and a feeding tube in her nose since she would be unable to feed for the time being. On the 3rd of July her chest tube came out and we were able to hold her for the first time. A few days later they replaced the IV in her arm with a picc line in her head, which is a more permanent IV that doesn't need replacing as often. For a brief time she was on CPAP, just to open her airway and help her breathe while recovering. Soon after, a video swallow test was done to make sure there were no holes in her esophagus and to verify that everything was healing well and no narrowing was occurring. The surgeon reported that the results were promising and we would be able to start feeding her.
In addition to a full recovery, in order for Kinsley to come home the doctors needed to see that she was gaining weight and taking full feedings every three hours by mouth without needing to use the feeding tube in her nose.
She started out strong, taking half of her feedings by mouth with the bottle, and latching at the breast like a champ. Often she would become exhausted halfway through feeding and fall asleep, so the remainder of her bottle (60-70%) was put in her feeding tube. Every time we fed her she tolerated the full feeding without spitting up. This went on for a few days until she stopped eating and was unconsolable. The doctors determined that she had acid reflux and started to give her Zantac to combat it. From there we had more success with feeding, all the way to the point that she was taking 50% on her own. At 80% the feeding tube can come out, and we were hopeful that we would get there soon.

Unfortunately, Kinsley began having episodes where she stopped breathing during feedings. Two times medical attention was required to bring her oxygen back up to safe levels. At that point, the neonatologist ordered that she been seen by the Occupational Therapist (OT), who came to watch her eat. On the 17th feeding by mouth was deemed unsafe due to oxygen desaturation and her color turning as a result.
OT ceased oral feedings and decided it best to have the Ears/Nose/Throat (ENT) doctor see her and order a new course of action. That evening ENT took a look at her throat and reported that her strider was one of the worst they'd ever heard, and there most definitely was extra floppy tissue blocking her airway.
Currently, ENT has ordered a 48 hour cease on her oral feedings to see if the swelling in her throat will go down so that they can do a bronchoscopy. Depending on the results of that test, ENT will determine with the pediatric surgeons whether or not the extra tissue will have to be surgically removed. It has been said that this is the most likely outcome. So, to recap, this is where we're at:
June 25- Kinsley is born
June 27- Surgery
June 29- CPAP
June 30- IVs out, Picc line in
July 2- Morphine stopped, CPAP off
July 3- Swallow Test, feeding began
July 6- Acid Reflux discovered, Zantac started
July 10- Taking 35% of feedings
July 14- Taking 50% of feedings
July 15/16- Stopped breathing
July 17- OT stopped oral feedings, ENT ordered Bronchoscopy
July 18- Surgery is being discussed
A second surgery means starting back at square one, where we began three weeks ago. Our daughter will be put under again, she will have a breathing tube and feeding tube, IVs will be replaced and a picc line will be put back in her head. We will be unable to hold her, unable to dress her, and she will have to learn to eat all over again after she recovers from this second surgery. All of the progress she has made will be erased.
The emotional burden is immense; maybe you know what it is like to live out of your backpack, miles from home- maybe you can remember a time where it took all your strength to get to the next minute of every day- it's possible that a stressful situation has robbed you of your appetite and sense of calm, among other things- and perhaps you can imagine what it is like to jump at the sound of your cell phone because every call could be the news that causes your undoing. It has been a long three weeks of this, and our journey is only just beginning.
These are all things Nick and I have been overcoming together. However, after three weeks off work, Nick has had to return to Petoskey to pay the bills, as our financial resources have been stretched to their limits. Now that he has had to return to work, we have to overcome these emotional struggles 200 miles apart, and on our own.
It has been a long three and a half weeks. We have recognized our need for help, and we feel it is now time to ask for it.
It is my hope that in sharing our story, by the kindness of people's hearts, the stresses of the financial burden can be lessened. Any donations made will help cover Kinsley's medical expenses not covered by insurance and the living costs such as food and a room for our extended stay at the hospital.
From the bottom of our hearts, we thank you for taking the time to read our story. We thank you for your positive thoughts, vibes, and prayers. If you are unable to contribute to the fund, please share our story with people you know, and continue to keep our sweet baby in your thoughts and prayers- she needs them now more than ever. We will get through this...she is refusing to sink.

Organizer
Miranda Lynn Byard
Organizer
Petoskey, MI