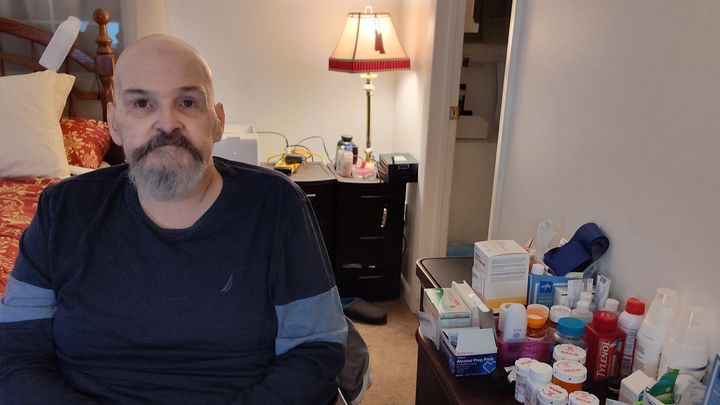
(Update) My Miracle Scott. I Need To Ask For Help
Donation protected
Update 05/16/2024
Scott finally had his colonoscopy on 05/15/2024. The doctors said that he’s healthy and will not need another colonoscopy for 10 years. All of the blood (and there was a significant amount of blood) was from the hemorrhaging from the nose. This bleeding sat on his stomach and ran through the intestinal tract. The bleeding was so heavy internally that it reduced his hemoglobin to 6.6. He’s been holding steady at 7.2. Still low but holding. He hasn’t had a transfusion since May 11th. His body is actually doing the work, which is good.
Scott had a bloody nose since the open-heart surgery on April 6th. (The actual bleeding from the nose slowed to a visual stop two days after he was admitted to Backus on May 6th). ENT at Hartford Hospital would not do a consult while he was in Hartford Hospital Rehab even though Dr. G had asked three times while Scott was in the Rehab portion of the Hospital (The Conklin Building, 6th Floor, a mere walk across an internal footbridge). Also, both Scott and I had asked repeatedly throughout his stay. The day before he was released from Hartford Hospital, ENT sent over some type of foam that was inserted into the nose but while this slowed the bleeding, it did not stop the bleeding.
After the colonoscopy on the 15th of May, Scott went into Rapid AFIB. His heart rate was up around 150. His BP was 78/44. He was struggling big time. No pain, but he couldn’t talk, He was trying to communicate but doing a great deal of word searching. He was lethargic and distant, he was struggling to stay focused. The Backus Staff of nurses were in his room with about three doctors in the mix as well. They calmed him down and stabilized him to an acceptable range of vitals. Granted they weren’t great, but he was stable. His heart rate stabilized at 119, and his BP came up to 99/65. The doctors got him calmed down enough so I could leave around 8:00 pm.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
May 16th, 2024:
This morning, I got a call from him at about 6:00, He needed me there to get through the interviews with the doctors because he could not talk. He’s doing a lot of word searching. He’s not doing well. He put in a pretty rough night. I went in at 8:00 am to see if I could catch the doctors on their rounds.
Scott saw Dr Peters (Nephrology / Dialysis). Dr Peters explained that the body jerking was due to the body being under stress and possibly dialysis. The cramping he’s experiencing could be from the dialysis solution not being at body temperature. The solution is supposed to be warmed to 98.6 at a minimum. The warmer that they have to warm the solution is not heating the solution to the minimum temp, but this is the second one they’ve used for him. The first one died altogether.
Scott saw Kevin Richards (Cardiology) while his vitals had been stabilized, Dr Richard stated that the actual heart surgery was doing fine he had no issues with how the heart was doing throughout the Rapid AFIB episode. Moving forward we will always have to watch Scott for AFIB activity because once you’ve had a stroke, the risk of having another one under Rapid AFIB will always be a concern. Dr. Richards was more concerned about another stroke more so than another heart attack.
Scott saw Wound Care for the open sores he has on his toes and leg area. They did a skin check to make sure that his skin was not breaking down anywhere else on the body because of the extended bed stay between Hartford Hospital (35 days) and Backus Hospital (as of this post, 9 days and counting).
Scott saw the floor doctor, Dr Chen. I don’t count her as support really, she’s a floor doctor and doesn’t really do anything but sign paperwork when Scott needs medicine adjustments. She knows nothing about Scott, his history, his trauma, she doesn’t even know his name half the time. I’m not impressed with this individual at all.
I’m still waiting for CT GI (Priscilla Quilters) to visit as of Friday, May 17th for follow-up information. But they haven’t stopped by yet.
The battle for today is Scott is now on day 6 of not eating. He stopped eating ice chips on Wednesday because everything he puts in his mouth makes him sick as a dog. He throws it all back up. He’s been doing dry heaves because he has nothing left to throw up. I’ve tried to coax him with ANYTHING he wants to eat. (At this point it doesn’t matter if he’s a diabetic, eating anything is a start). I’ve tried chicken broth, pizza, cheeseburgers, pies, cakes, cookies, chicken Mc Nuggets, milkshakes, and protein drinks, He won’t even entertain sipping coffee…. something we used to love to do together. Just enjoy each other’s company over a cup of coffee. Today he promised me that he would try to eat some oatmeal. Wish us luck.
May 9th, 2024:
Scott was visited by Dr Lail, Navdeep Singh, MD, After an MRI of the neck and head. Dr. Lail showed Scott and I the MRI and determined that Scott had had a “recent old” stroke in the front right cortex of the brain, probably caused by the Rapid AFIB he had experienced after the heart surgery while in Hartford Hospital (for the record, no they did not do an MRI at Hartford when he had Rapid AFIB, only a chest X-Ray). This stroke is affecting his speech. While he can visualize the word he wants to use, he cannot say it. The doctor explained that this tissue was dead, and there was no use going back to try and reactivate it. But what we can do, is work with the surrounding tissue. The surrounding tissue should take on the personality of the dead tissue and his speech will return in time. However, if Scott is under any type of stress his speech will diminish and he will struggle with “word searching”. Also, any stress will run the risk of throwing him into Rapid AFIB again, once a person has had a stroke, and goes into Rapid AFIB, the possibility of having a stroke is high.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
Update as of 05/12/2024:
Well.... Now, we’re looking at the possibility of peritonitis. The doctors are running tests to see if Scott may have peritonitis. What is peritonitis? Infection is the most common cause of peritonitis, and it can be very dangerous. Symptoms of peritonitis include belly pain or tenderness. Bloating or a feeling of fullness in the abdomen and fever.
Scott has been living off ice chips for the past two days. He hasn’t eaten anything today or yesterday. He says he feels pressure and bloating. He can’t stomach food right now. When they bring in his dinner tray, it causes a gag reflex. I’ve tried bringing food in from outside of the hospital, only to throw it away without being touched. He won’t even eat Jell-O now.
They have Scott on an antibiotic cocktail to try to cover all possibilities until they can determine specifically what is going on.
Also, Scott is struggling to find the right word when he carries on a conversation. He will have an MRI of the head and neck area this evening to determine if there may be something going on with the brain.
The plan is to move forward with an endoscopy and colonoscopy tomorrow to figure out where the bleeding is under twilight sleep, once located, they will try to use Electrocauterization on the bleed. I’m praying for an ulcer and not something……more serious.
For tonight, Scott is still at Backus, doing manual drip dialysis, receiving antibiotics, and MRIs, and waiting to hear about what time he’ll be going down for his procedure.
Please pray for us. We could use the light of hope and maybe a miracle or two.
Thank you to everyone who has supported us through this overwhelming time in our journey. I can’t tell you what it means to have you there.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
Thursday, May 9th, 8:30 pm
Update II:
Scott FINALLY got a private room at 1:50 this afternoon. While in the ER, Scott received a consultation from Connecticut GI regarding doing a colonoscopy to find out where the internal bleeding is coming from. The doctor reviewed Scott’s medical history from this last open-heart surgery and noted that he was having lung spasms from the heart surgery. She explained that right now, a colonoscopy would be risky right now because Scott would not tolerate anesthesia. His lungs wouldn’t fare well. She would have to find another solution. She had mentioned several options but wanted to consult with her peers to find the best possible path for Scott.
As of 8:00 this evening Wound Care did not come to look at the open sores on Scott’s toes. I’m hoping tomorrow they will show. I’ll cut them some slack because Scott never got to his room until 2:00 this afternoon. But tomorrow… “We’ll talk” if they don’t show.
Scott received another transfusion and another cycle of dialysis. He got sick over supper so he hasn’t eaten much today, but his diabetic sensor states he’s in range and doing ok. They gave him some Zofran for his upset stomach. His only complaint tonight is that he’s cold. (In his defense the room is cold). The nurses said the room he has is always cold, so they gave him warm blankets.
It’s been a long 48 hours. We’re both exhausted and a little overwhelmed right now. But he’s safe, he’s comfortable, he’s loved, we’re ok.
With all of this being said, our plans have changed. I will have to take an extended leave of absence from work to take care of Scott. The future is scary looking right now. We’re both so tired…..but…full of hope. Even in the darkest of times, there will always be the soft light of hope.
Please understand, that I’m so exhausted I can’t see straight right now, but I want to take the time to say Thank you for helping us through this incredibly difficult time with paying insurance premiums, food, gas, medical co-pays, supplies, bills, medical equipment, keeping the lights on, and the rent paid through this battle. It’s all been so very overwhelming for us. I’m not sure I could stand it if I didn’t know that you were with us. Please know that If you are unable to help us financially, love and prayers are most welcome. Scott is my miracle. Miracles are born through the power of prayer…… Thank you so very much for your support and your love.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
Update May 8th, 2024:
Scott came home (after a very long 35-day stay at Hartford Hospital) on Monday, May 6th. He was very frail, but home. He had a continuous bloody nose, and Scott had admitted to me that he had blood in his stool but wanted to address it at home. (This would be our downfall). He was weak as a two-day-old pup, but happy to be in his own space.
Scott came home with all new prescriptions which total $480.00 in co-pays, and one is still out for authorization with the insurance because our co-pay on that one will be $600.00. (There is no generic to counteract the high cost of the drug). Please let me take a moment to acknowledge the fact that I could not have picked these up without your financial support. THANK YOU!
Scott got in one good night on peritoneal dialysis. The home dialysis took off 786 ml of fluid and his lung spasms went down to a minimal amount. He slept in for a little while peacefully, but this bubble of peace didn’t last long….
On Tuesday afternoon, May 7th, we had an appointment with DiVita (Dialysis). They drew blood and called us Wednesday morning. Scott’s hemoglobin was down to 7.0. This is the point where everyone screams “The sky is falling”. He had to report to the ER at Backus Hospital here in Norwich to receive a transfusion.
We got to the hospital around 11:00 am. He was sent to the ER and “processed” for a blood transfusion. More blood was drawn. A really alert and brilliant young doctor named “Alex” was Scott’s doctor for this visit. He came into the room and apologized for taking so long to meet with Scott. He had explained that he took the time to read Scott’s medical history. I’ve NEVER had a doctor say this before. Scott’s medical history is the size of the Britannica encyclopedia hard copy series. Doctors usually just look at the patient in the bed and look at what’s in front of them. They don’t care about the history or the trauma of what the body has been through…… I took a breath for the first time in 6 weeks…
“Alex” immediately explained that Scott’s hemoglobin had shot down to 6.6 and he would be admitted. Alex said, “Scott please understand, this is way too scary for just a blood transfusion; your medical history is too extensive, and something is happening inside; we have to find out what that might be”. Scott explained to the doctor that he had been battling a bloody nose for about three weeks in Hartford Hospital with only ONE visit from ENT (Ear, Nose, and Throat) two days before he was released. It seems the ENT did not want to bother Scott because he was in the Acute Rehab ward of the hospital and not the actual hospital part, even after THREE requests from Scott’s doctor to consult, (this is partially why Scott wanted to come home. He would get more help on the outside than in the hospital from ENT to address the bloody nose). Also, Scott said he had “A LOT” of blood in his stool and that would explain what was happening. The doctor did a rectal exam in the ER and found blood. The color of the blood was a dark garnet/burgundy color. Alex said this was serious and this would need a colonoscopy to find the actual cause of what was going on inside. It was a significant amount of bleeding.
Alex explained that bright red blood in your stool usually means the bleeding is lower in your colon, rectum or anus (not the case here), Dark red or maroon blood can mean that you have bleeding higher up in your colon or your small intestine. “Melena” (black stool, kind of looks like coffee grounds) often points to bleeding in your stomach, such as a bleeding stomach ulcer (again, not the case here). Scott’s in trouble.
Alex gave him a blood transfusion in the ER and this brought his hemoglobin up to 7.2. his blood pressure went up from 77/44 to 108/58. Also, he received a manual drip dialysis in the ER. All of this seems to have stabilized him for the night.
Scott sent me home at 11:00 pm because there were no beds available. He would spend the night in the ER until discharges took place this morning to give him a private room. (he is still in the ER this morning, and he must wait because he has too many things going on to share a room apparently).
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
May 6th, 2024:
I’m so very tired. I’ve never felt so overwhelmed, I don’t know how to do this. I need to ask for help, but it goes against every grain of who I am.
Some of you may or may not know that Scott has been in Hartford Hospital this past month because of open heart surgery. It’s been a long road, and we’re not out of the woods yet.
I have had to take days off to run to the hospital and now I need to take a (we’re starting with at least two weeks, maybe more) two weeks leave of absence to support Scott while he comes home (which was originally scheduled for Friday, but we had to push it out to this coming Monday while The Team tries to address fluid on the lungs and heart AFib, and low BP).
Scott has a medical history the size of War and Peace. He started out with blood clots in his late teens, and then it went downhill from there:
1. Polycythemia vera (blood clotting disorder usually found in people over 65 years old.
2. (3) bouts of Acute Myeloid Leukemia (known as AML).
3. Two bone marrow transplants (one in 2004 and then in 2007)
4. Pyoderma gangrenosum: (in Scott’s case, it’s a Graph Vs. Host disorder from the bone marrow transplant), This is a rare condition that causes large, painful sores (ulcers) to develop on your skin, most often on your legs. The exact causes of pyoderma gangrenosum are unknown. It appears to be a disorder of the immune system.
5. Scleroderma: (in Scott’s case, it’s a Graph Vs. Host disorder from the bone marrow transplant), This affects many parts of the body. This is the more serious form of the condition. Without intervention, it may become serious and life-threatening.
6. In 2019 Scott had a heart attack (called the infamous “Widow Maker”. He had an artery that was 90% blocked and another that was 75% blocked. The doctors said he was “a dead man walking”.
7. 2021: Scott spent from February through Late August in the hospital with Osteomyelitis. Osteomyelitis is a severe bone infection caused by bacteria or fungi. It causes painful swelling of bone marrow, the soft tissue inside your bones. Without treatment, swelling from this bone infection can cut off the blood supply to your bone, causing the bone to die.
a. After this particular hospital stay with the Osteomyelitis, Scott would become a dialysis patient and an amputee patient, The medicines they provided to save his life also weakened the heart which was already exposed to the strain of chemotherapy and radiation treatments (see 2019 Widow Maker under 6.).
b. Scott was in a coma for 2 ½ months, the Osteomyelitis infection went into his brain, his heart, his lungs, his liver, kidneys, and pancreas. He coded twice.
c. The medicine that they provided to save his life destroyed his kidneys. Scott is now a dialysis patient.
d. While battling Osteomyelitis, and because of the damage done to the right leg, Scott had to have the right leg amputated to save his life. The Team did a biopsy on the amputated leg and found Squamous cell carcinoma. (CANCER)
Squamous cell carcinoma can grow large or spread to other parts of the body. The growth of the cancer caused serious complications.
e. Because of this cancer find, they had to go back in and amputate above the knee to make sure they got all of the cancer markers.
f. Scott had to learn how to talk, write, type, and do critical thinking all over again after he woke up from the coma when battling Osteomyelitis.
8. In 2024 Scott went to the hospital on March 30th with chest pains. He had a blockage of 75% and damage to the left ventricle of the heart. They could not stunt this artery because of where the damage was on the heart. The damage was where the left and the right ventricle split to provide blood to the heart. He had to have open heart surgery. Scott’s veins in his legs were too scarred from old blood clots (from the Polycythemia vera and the hardness from the Scleroderma).. His veins in his arms were too small and too scarred because of all of the IVs, blood draws, old blood clots, etc. They had to use the Mammary arteries on either side of the chest wall. They placed one in the front of the heart and one in the back of the heart to bypass the damaged left ventricle and other damage found on the heart.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
May 5th ,2024:
Scott was scheduled to come home this Friday, May 3rd, but they cannot stabilize his blood pressure, (1) 51/44, (2) 81/44, (3) 70/40 etc.) They cannot get it to come up and then stabilize.
Scott is also experiencing RAPID AFIB; His heart rate has been very high. It’s coming down but it’s still concerning.
He is bouncing between low-flow O2 and room air. He’s mostly room air at this point.
He has fluid on the lungs and heart, (minimal, but still present), The Team said it’s the heart protecting itself from all of the stress the fluid is a protection phase from the surgery, which is backfilling into the lungs.
Scott is now a medically induced diabetic now because his body is under so much stress and the meds they have him on.
The team is trying to stabilize him long enough to get him home so we can start the healing portion of this latest journey. He cannot be alone while he’s home. I have to be with him 24/7.
Scott and I need help paying incredibly large medical bills, prescriptions co-pays, gas for hospital/doctor visits, and medical equipment and supplies that insurance won’t cover..... There’s just so much debt and future debt that I can’t handle alone. I need to swallow my fear and my pride and ask for help with humility. If you can help us financially, I can’t thank you enough.
If you can’t help us financially, I understand but we can use prayers. As you can see, Scott is my miracle, he’s “my person”. I will fight to the death for him. Prayers are most welcomed.
To all of you, Thank You for being with us on this incredibly overwhelming journey. We could not be here without your love, your prayers, and all of you holding us in the darkest of times. Scott and I know you’re there.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
Organizer
Lynette Devlin
Organizer
Norwich, CT