Please help!! Our Dad, Don Williams, is trapped in a rare condition called Locked-In Syndrome after suffering a massive stroke 3 months ago.
He has always been a very active person who is never sick, has no chronic conditions, and needs no prescriptions---and if you met him you would think that he is 20 years younger than he is, not only because of his appearance and activity levels, but also due to his sharp wit and intellect.
Sadly, on April 29, he suffered a massive stroke and quickly went into Locked-In Syndrome, a very rare, horrific neurological condition in which he is fully aware of what is going on around him, has all of his cognitive abilities, memories, etc., and can feel all physical sensations, but is unable to speak or move anything, except for his eyes, which he can only move vertically, up and down. The only way he can communicate is to answer Yes/No questions by raising his eyes up for “yes” or down for “no”.
Meanwhile, COVID-19 rages on, bringing additional challenges. We fight for the barest of visitation rights for Mom to visit him, so that she can bring him love and support, play recorded messages from all of us, and encourage him toward his recovery. Imagine how it feels to be "locked in"---frightened, confused re: what has happened to you, unable to move, scratch an itch, express yourself or ask for help---and then on top of that, unable to have your family, or anyone you know, around you for support! COVID has truly made this a DOUBLE TRAGEDY.
As time passes and his situation progresses, our family is increasingly desperate for Dad to receive the required treatment necessary to recover from his ordeal and find his voice.
Everything we have read about Locked-In Syndrome says that with fast intense rehabilitation there is a better chance of recovery, but we are struggling to do enough with his insurance-approved care levels. I'll get to that later, though, and keep to the positive. More detailed info about our journey to-date can be found below in the “What Has Happened” section. We'll also provide updates as time goes on.
Dad’s Accomplishments To-Date
In just over three months, Dad has graduated from the ICU and moved on to two different facilities, where he has worked hard to not only get off of the ventilator, which he accomplished in June (only 50% of locked-in patients get off of the ventilator! Go Dad!!), but to also gain movement in other parts of his body.
So far, he has achieved several things:
· quicker response times on questions (with his vertical eye movements of up for "yes" and down for "no"); improved from 9 seconds down to 1 or 2 seconds;
· regaining some horizontal (left/right) eye movements, which will enable him to use letterboard to communicate (versus only yes/no questions);
· moving his fingers in Mom's hand, then improving over time to lightly "grasp" her hand, i.e. bringing fingers and thumb together;
· spelling out multiple words and answering simple questions using the letterboard; and
· moving his head to the side, and even holding his head up by himself
All of this is great progress that shows how much of a FIGHTER he is…once a Marine, always a Marine! However, he has a long way to go (and a short time to get there), with only 100 days of insured rehab available, of which we’ve used about 35 days at July 29. In addition, the Speech, Occupational, and Physical Therapy that he receives is only 30 mins per day, 5 days per week. When you add those things together, his coverage is just NOT ENOUGH---neither in its intensity nor its duration---to be the “fast, intense” rehabilitation that everything we’ve read says is necessary in order to recover from Locked-In Syndrome.
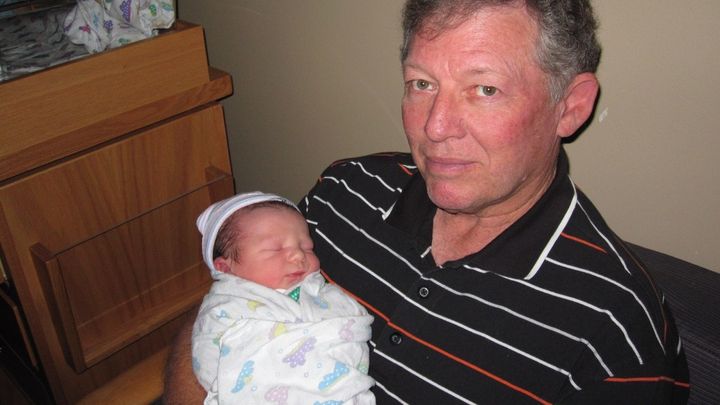
 Dad...a new Grandpa.
Dad...a new Grandpa.
Our Proposed Plan – Where We Need Your Help
He will need long term care and support, including a variety of intensive rehab therapies. We want to include NEUROLOGICAL rehabilitation, but Dad’s insurance states that type of rehab is “not medically necessary" (what?!).
Since Dad's insurance won't help, these extra rehab expenses would be full cost to him and Mom, for which their incoming Social Security benefits are insufficient. In fact, after receiving a quote of $1,600 per day for 1:1 in-patient rehab services at a neuro-rehabilitation facility that specializes in brain injury, we calculated that only 6 months of rehab would cost $292,000...6 MONTHS!!!
It is a massive amount, but even if we can only provide him with 6 months of the specialized care he needs, it will help to kick-start his recovery. With any additional funds, we can decide to increase his months at the neuro-rehab facility (12 months would be a better goal) and/or we can use any funds raised through this effort for the following additional expenses:
· to pay medical bills and hopefully improve care options in other ways. Depending on how well he recovers in the short term, there will be longer-term needs, including expenses...
· to hire help for my Mom to care for him at home upon his release to her care (after only 100 days? Give me a break!), like a nurse or rehabilitation therapists
· to obtain a wheelchair once he is able to control his body enough to use it;
· to do home modifications to accommodate a wheelchair and/or install other equipment needs (a lift?) that may become necessary over time;
· to perform car modifications, or rent / purchase a vehicle (or use a service?) as a medical mobility option to get him to doctor appointments and other needs;
· to incorporate technology-enabled aids / tools to facilitate his recovery and improve his communication, his physical abilities and his quality of life.
In the meantime, though, we feel that the need for more rehab comes first, especially incorporating neuro-rehab. The level of success he achieves with this rehab will determine how much he will need in the long term (example: if he can come out of neuro-rehab WALKING, then he won't need a wheelchair!).
We had honestly never thought about asking for help on the Internet, but a close friend of the family suggested we create a GoFundMe page to ask family, friends, and others to help. So, we’ve taken our first stab at it here and hopefully we've done a good job. Yes, we have such a large goal that it seems overwhelming---believe me, we know---but anything you can contribute will be more than we have today and would be helpful and appreciated!
Please pray for him and my mom, too! She is having a hard time and the constant insurance battles have made it harder for her to keep her faith and stay positive.
And, finally, if you know of someone else in a similar situation, or if you have heard of any people doing positive things in neurology or rehabilitative therapies or technologies, including any clinical trials that we should look into, then please let us know and forward this information to them. Any thoughts, advice, contacts or referrals would be welcomed!
Dad is ready for this challenge - he proves that every day!! We are ready, too! We promise to give you updates on his recovery, and how any funds are used, as we move forward.
Thank you from the bottom of our hearts!
About Dad

Our Dad, Don Williams---"no, not THAT Don Williams" (the singer), as he always jokes---was born in Florida and grew up in Steinhatchee and Jacksonville before marrying our Mom at the age of 22. He was a Marine during the Vietnam War era. He joined the technology industry as a Systems Analyst, and he and our growing family moved a lot over the first 12 years of their married life, living in Minneapolis, Fairfax, VA, Los Angeles, Oklahoma, and Merritt Island, FL (Dad worked w/ NASA at nearby Cape Canaveral) before settling in Texas for the past 40 years in the areas of Austin and San Antonio.
Dad is a beloved husband, father, and grandfather. He is very smart and has a sharp wit. He loves to throw out clever puns, one-liners, and movie quotes and, at most family functions---back when they occurred (thanks COVID-19!)---keeps all of us laughing and trying to win the pun-off!
He is very active, with a love for life, golf (with a 68 handicap!!), and the great outdoors (he loves to go for drives in the countryside).
He is a friend and mentor to many, and an enemy to none.
 Dad and Mom, hanging with their grandson at the Wildflower Center in Austin
Dad and Mom, hanging with their grandson at the Wildflower Center in Austin
What Has Happened
** This section is detailed because I believe that others can learn from Dad's experience, and from our experience dealing with his insurance providers, as well as his doctors and other caregivers. **
The Original Incident & ICU
April 19 to 27 - After a few bouts of dizziness and nausea that would come and go, Mom and Dad checked the Internet, checked Dad against a list of stroke symptoms they found, and then concluded that he must have an inner ear issue. But then he began having a few vision and hearing oddities, so they finally went to a clinic despite their nervousness about COVID-19 (at this point, they had already been homebound for several weeks).
April 27 to 29 - Dad was transferred to an area San Antonio hospital for 2 days of tests and observations. An MRI showed that he had experienced a TIA (Transient Ischemic Attack) or "mini-stroke", which surprised Mom and Dad, since he'd had no physical or mental effects that would signal a stroke. In fact, he continued to walk around and have calls with friends and business colleagues during those days at home and then during his time in the hospital as they tried, unsuccessfully, to determine the cause of his TIA. We heard later that he was hardly ever in his hospital room, and that the doctors and staff really enjoyed him at the hospital…Dad has a sharp wit and is a funny guy!
April 29, 2020 - On Dad's last planned night in the hospital, he had a massive stroke in the area of the brainstem that controls, among other things, involuntary (survival) functions of the body---breathing, swallowing, heartbeat, etc. They intubated him and put him on a ventilator. We were shocked, as were the doctors and nurses that had seen him so active and engaging during his time there.
April 30 - May 1 - Dad's doctors and caregivers must have realized that Dad was "in there" because they diagnosed him with Locked-In Syndrome, a rare condition in which he is fully aware, with full cognitive functions, memories, etc., but is paralyzed, unable to speak or move (with the exception of vertical eye movements). We were horrified upon learning about it.
April 30 - May 6 - During this first week, Mom and our brother Stephen, who also lives in San Antonio, received special permission from the hospital to visit him in the ICU, where he was sedated and on a ventilator. The hospital was NOT allowing visitors due to the COVID-19 pandemic and we learned later that they only gave permission because they thought he wouldn't survive.
This first week, we were asked to make a heartbreaking decision...either take him off of life support, in hospice care, sedated, and unaware of what had happened, or do two surgical procedures to give him more time: a tracheostomy (breathing tube in his throat) and a PEG (Percutaneous Endoscopic Gastrostomy) feeding tube. We knew that he had told Mom multiple times that he didn't want to be on a feeding tube, like his Grandmother, but we didn't know if he'd feel the same now. Bringing him out of sedation to make his own decision was a good idea, but that would also make him more aware of his situation and the doctors' prognoses were dire. They warned us that giving him more time didn't mean he would recover. Many people die because they don't come off ventilator successfully, or they have complications like blood clots, pneumonia from lying in bed. We were also on a heartbreaking rollercoaster ride with a variety of his doctors (many recommending the hospice route)---first we go up, with good news from his respiratory doctor that Dad was "over-breathing" the respirator (doing some breathing himself)---yay, Dad!---then the next day, we go down, with a palliative care doctor telling us about end-of-life options---boo!-- We were crushed.
May 6 - 8 - On the afternoon of May 6, Dad was brought out of sedation enough so that a doctor could tell him his prognosis and allow him to make the decision himself. Multiple doctors visited him over the next day or two to explain what had happened to him, to give him their perspectives, and to have him repeat his yes/no answer. Mom and Stephen also visited to ask him questions to test his memory and cognitive skills and to make sure he knew that we were with him no matter what! Each and every time, Dad chose to have the two procedures and take on the challenge! That’s our Dad! He is a fighter and we are so proud!!!
May 12 to 13 - Dad had the trach and PEG procedures performed and sailed through post-op recovery.
May 21 - Dad was discharged and transferred to Post-Acute Medical ("PAM") specialty hospital in New Braunfels for the next step in his recovery.
Dad's Ongoing Recovery (and Insurance Battles)
May 21 - June 24 - Dad was at PAM---a small hospital w a focus on respiratory issues and weaning patients off of ventilators. During these 6 weeks, he not only came off of the ventilator (achieved by only 50% of locked-in patients), but also twice had his trach tube reduced in diameter with no issues. This was a great success! Either Mom or Stephen could visit him EVERY DAY to give him love and support, bring him our audio and video messages, read to him, and hold his hand.
June 21 - with COVID-19 numbers rising over the previous weeks in Texas, due to its early open in May, the governor had to re-lock down healthcare facilities, and Mom could no longer visit Dad at PAM. This new lock down was especially difficult because we were told that Dad needed a new facility to move to by the end of that week. This meant we had to find a new facility for him, all without the ability to tour potential sites or meet with them in person!! All we could do was Internet research and phone interviews and hope for the best!
June 25 - Dad was moved to a Skilled Nursing Facility (SNF) for skilled nursing (trach, PEG and catheter) and rehabilitation services. The first two weeks were hard because the facility didn't have all of the equipment he needed and Mom couldn't visit him...all she could do is speak with people over the phone to check on him and tell people about his special condition and his equipment needs. Key people responsible for his care wanted to write him off and she had to tell them that "he is in there", what Locked-In Syndrome is, and what it means for his care. These early conversations and equipment delays did NOT help us believe that we had made the right decision!
July 6 - Finally, Mom could visit Dad, after getting a negative COVID test. She helped inform his caregivers and showed him our videos and encouraging messages.
July 14 - On this Tuesday, she came for a second visit and noticed that they finally had a good set-up in his room! She was approved for Tuesday/Friday visits and we were thankful that she could go 2x per week to check on him, participate in his care, and support him. All of his therapists told her that he was much more alert and focused when she was there and concluded that her visits are critical. By now, Dad's progress included moving his fingers in Mom's hand and working with his therapist to move his eyes laterally, instead of just up and down. Enter Dad's insurance providers, to "take care of" (destroy) all of those good feelings...
July 16 - After ONLY THREE WEEKS of skilled nursing and rehab at this facility, Dad's insurance providers, UnitedHealthcare and WellMed, handed down a decision to DISCHARGE Dad from care as of Monday, July 20 (even though he would only be in day 25 of the 100 days of skilled nursing and rehabilitation that is in his freaking policy)! Mom had until 12:00 pm noon on Saturday, July 18, to appeal this shocking decision. Mom wrote a long, handwritten statement and faxed it to the QIO, Quality Improvement Organization, a special 3rd party org that handles appeals. Over the next several days, Mom had to do this same appeal process two additional times (as did the QIO) because the facility didn't submit their clinical records to the QIO in time. Grrrr...
July 24 - Third time lucky! Dad's facility must have submitted their paperwork this time because Mom learned that the QIO had approved our appeal, determining that Dad's skilled nursing and rehabilitation were necessary. Such great news! Meanwhile, Dad had more improvements, like successfully moving his eyes from side to side. He is now ready to use a letter board to spell out words, instead of just answering yes/no questions with up/down eye movements. Yay! Mom also noticed him beginning to move his lips, tongue, and even swallow. This could mean that he may soon be ready to relearn his mouth control for breathing and swallowing, enabling future removal of the trach and PEG. He also "grasped" her hand multiple times, lightly bringing fingers and thumb together.
July 30 - Only 6 days after Dad's care is deemed necessary, ANOTHER DISCHARGE ATTEMPT is filed and needs to be appealed. Didn't we just do this??! Will we have to do this every 6 days? Really?? Mom had until noon THE NEXT DAY to fax in another statement. Since it'd only been 6 days, she faxed in the same statement. In the meantime, The facility is supposed to send in their clinical records. Hopefully, they remember to do this because Mom is spending $$ to send faxes from the UPS Store (they have no home phone). Four faxes so far!
August 1 - Appeal is DENIED because he hasn't shown enough progress. What? This past week, Dad has spelled several words on the letter board, has tracked with his eyes, has moved his head sideways, and has even held up his own head. HOW IS THAT NOT PROGRESS?? We are told to write a "Family Letter of Concern" and fax it in for "reconsideration" of the denial. We also got letters from his rehabilitation therapists for PT, OT, and ST stating that Dad needs their services, as well as skilled nursing, and sent it all on Sunday night, August 2nd.
And, now, we wait...(any later updates will be entered in "Updates" section)
We will continue to fight for Dad to not only receive his full 100 days of benefits (which are abysmal anyway, compared to the many months to a year of rehabilitation therapy that he will probably need), but also to receive some CONTINUITY of care, with a group of therapists and nurses that he knows and trusts! He can’t keep moving from site to site every few weeks, as soon as we have a great team of caregivers working with Dad and fighting alongside him.
Please pray for our Dad!
Locked-In Syndrome – What Is It Like?
Locked-In Syndrome (LIS) is a rare condition that few seem to understand in the medical community. At first, most locked-in people are thought to be in a vegetative state, since they are motionless and have to be put on life support systems, like ventilators and feeding tubes. Later, someone---many times, a family member, but it can also be a doctor or caregiver---recognizes that the patient is present and aware, which leads to an LIS diagnosis.
There are several articles, books, and videos out there that tell the story of what it is like to be locked in. These people are at varying points in their recovery from LIS and have different ways of communicating---blinking, letterboards, or speaking---but all have been able to tell their story in their own words:
1. Voicing Inner Thoughts Matters | TEDx - Talk given by Kate Allatt, who had a brainstem stroke and LIS, started the site fightingstrokes.org, and wrote 3 books.
2. Breaking out of Locked In Syndrome with Richard Marsh - an article about a retired California police officer who suffered a brainstem stroke and LIS. See an interview of him here on YouTube . He also wrote a book called Locked In: One Man's Miraculous Escape from the Terrifying Confines of Locked In Syndrome.
2. How My Mind Came Back to Life and No One Knew | TEDx - Talk delivered by Martin Pistorius using speech synthesis, a form of Augmentative and Alternative Communication. Martin suffered a childhood illness at 12 that devolved into Locked-In Syndrome. He has also written a book called Ghost Boy.
3. The Diving Bell and the Butterfly - a best-selling book by Jean-Dominique Bauby, Editor-in-Chief of Elle Magazine who suffered a stroke and LIS in 1995; the book was made into an award-winning movie of the same name in 2007.
4. The Patient's Journey: Living with Locked In Syndrome - an article on the National Institute of Health (NIH) website from the point of view of Nick Chisholm, who suffered a traumatic injury during a rugby game which led to stroke and LIS.
#LockedIn #Locked-In #LockedInSyndrome #Locked-InSyndrome #Help #StrokeSurvivor #TBI #BrainInjury #Stroke #StrokeRehabilitation #StrokeEducation #StrokeAwareness #Health #TeamDon #FightForTeamDon #Fight4TeamDon #Don'sVoice #DonsVoice #Veteran #Marine #Health #Recovery #Rehab #NeverGiveUp #StillMe #Neurorehabilitation #BrainStem #Paralysis #Aphasia #Disability #Physiotherapy #SpeechTherapy #Neurology
He has always been a very active person who is never sick, has no chronic conditions, and needs no prescriptions---and if you met him you would think that he is 20 years younger than he is, not only because of his appearance and activity levels, but also due to his sharp wit and intellect.
Sadly, on April 29, he suffered a massive stroke and quickly went into Locked-In Syndrome, a very rare, horrific neurological condition in which he is fully aware of what is going on around him, has all of his cognitive abilities, memories, etc., and can feel all physical sensations, but is unable to speak or move anything, except for his eyes, which he can only move vertically, up and down. The only way he can communicate is to answer Yes/No questions by raising his eyes up for “yes” or down for “no”.
Meanwhile, COVID-19 rages on, bringing additional challenges. We fight for the barest of visitation rights for Mom to visit him, so that she can bring him love and support, play recorded messages from all of us, and encourage him toward his recovery. Imagine how it feels to be "locked in"---frightened, confused re: what has happened to you, unable to move, scratch an itch, express yourself or ask for help---and then on top of that, unable to have your family, or anyone you know, around you for support! COVID has truly made this a DOUBLE TRAGEDY.
As time passes and his situation progresses, our family is increasingly desperate for Dad to receive the required treatment necessary to recover from his ordeal and find his voice.
Everything we have read about Locked-In Syndrome says that with fast intense rehabilitation there is a better chance of recovery, but we are struggling to do enough with his insurance-approved care levels. I'll get to that later, though, and keep to the positive. More detailed info about our journey to-date can be found below in the “What Has Happened” section. We'll also provide updates as time goes on.
Dad’s Accomplishments To-Date
In just over three months, Dad has graduated from the ICU and moved on to two different facilities, where he has worked hard to not only get off of the ventilator, which he accomplished in June (only 50% of locked-in patients get off of the ventilator! Go Dad!!), but to also gain movement in other parts of his body.
So far, he has achieved several things:
· quicker response times on questions (with his vertical eye movements of up for "yes" and down for "no"); improved from 9 seconds down to 1 or 2 seconds;
· regaining some horizontal (left/right) eye movements, which will enable him to use letterboard to communicate (versus only yes/no questions);
· moving his fingers in Mom's hand, then improving over time to lightly "grasp" her hand, i.e. bringing fingers and thumb together;
· spelling out multiple words and answering simple questions using the letterboard; and
· moving his head to the side, and even holding his head up by himself
All of this is great progress that shows how much of a FIGHTER he is…once a Marine, always a Marine! However, he has a long way to go (and a short time to get there), with only 100 days of insured rehab available, of which we’ve used about 35 days at July 29. In addition, the Speech, Occupational, and Physical Therapy that he receives is only 30 mins per day, 5 days per week. When you add those things together, his coverage is just NOT ENOUGH---neither in its intensity nor its duration---to be the “fast, intense” rehabilitation that everything we’ve read says is necessary in order to recover from Locked-In Syndrome.
 Dad...a new Grandpa.
Dad...a new Grandpa.Our Proposed Plan – Where We Need Your Help
He will need long term care and support, including a variety of intensive rehab therapies. We want to include NEUROLOGICAL rehabilitation, but Dad’s insurance states that type of rehab is “not medically necessary" (what?!).
Since Dad's insurance won't help, these extra rehab expenses would be full cost to him and Mom, for which their incoming Social Security benefits are insufficient. In fact, after receiving a quote of $1,600 per day for 1:1 in-patient rehab services at a neuro-rehabilitation facility that specializes in brain injury, we calculated that only 6 months of rehab would cost $292,000...6 MONTHS!!!
It is a massive amount, but even if we can only provide him with 6 months of the specialized care he needs, it will help to kick-start his recovery. With any additional funds, we can decide to increase his months at the neuro-rehab facility (12 months would be a better goal) and/or we can use any funds raised through this effort for the following additional expenses:
· to pay medical bills and hopefully improve care options in other ways. Depending on how well he recovers in the short term, there will be longer-term needs, including expenses...
· to hire help for my Mom to care for him at home upon his release to her care (after only 100 days? Give me a break!), like a nurse or rehabilitation therapists
· to obtain a wheelchair once he is able to control his body enough to use it;
· to do home modifications to accommodate a wheelchair and/or install other equipment needs (a lift?) that may become necessary over time;
· to perform car modifications, or rent / purchase a vehicle (or use a service?) as a medical mobility option to get him to doctor appointments and other needs;
· to incorporate technology-enabled aids / tools to facilitate his recovery and improve his communication, his physical abilities and his quality of life.
In the meantime, though, we feel that the need for more rehab comes first, especially incorporating neuro-rehab. The level of success he achieves with this rehab will determine how much he will need in the long term (example: if he can come out of neuro-rehab WALKING, then he won't need a wheelchair!).
We had honestly never thought about asking for help on the Internet, but a close friend of the family suggested we create a GoFundMe page to ask family, friends, and others to help. So, we’ve taken our first stab at it here and hopefully we've done a good job. Yes, we have such a large goal that it seems overwhelming---believe me, we know---but anything you can contribute will be more than we have today and would be helpful and appreciated!
Please pray for him and my mom, too! She is having a hard time and the constant insurance battles have made it harder for her to keep her faith and stay positive.
And, finally, if you know of someone else in a similar situation, or if you have heard of any people doing positive things in neurology or rehabilitative therapies or technologies, including any clinical trials that we should look into, then please let us know and forward this information to them. Any thoughts, advice, contacts or referrals would be welcomed!
Dad is ready for this challenge - he proves that every day!! We are ready, too! We promise to give you updates on his recovery, and how any funds are used, as we move forward.
Thank you from the bottom of our hearts!
About Dad

Our Dad, Don Williams---"no, not THAT Don Williams" (the singer), as he always jokes---was born in Florida and grew up in Steinhatchee and Jacksonville before marrying our Mom at the age of 22. He was a Marine during the Vietnam War era. He joined the technology industry as a Systems Analyst, and he and our growing family moved a lot over the first 12 years of their married life, living in Minneapolis, Fairfax, VA, Los Angeles, Oklahoma, and Merritt Island, FL (Dad worked w/ NASA at nearby Cape Canaveral) before settling in Texas for the past 40 years in the areas of Austin and San Antonio.
Dad is a beloved husband, father, and grandfather. He is very smart and has a sharp wit. He loves to throw out clever puns, one-liners, and movie quotes and, at most family functions---back when they occurred (thanks COVID-19!)---keeps all of us laughing and trying to win the pun-off!
He is very active, with a love for life, golf (with a 68 handicap!!), and the great outdoors (he loves to go for drives in the countryside).
He is a friend and mentor to many, and an enemy to none.
 Dad and Mom, hanging with their grandson at the Wildflower Center in Austin
Dad and Mom, hanging with their grandson at the Wildflower Center in AustinWhat Has Happened
** This section is detailed because I believe that others can learn from Dad's experience, and from our experience dealing with his insurance providers, as well as his doctors and other caregivers. **
The Original Incident & ICU
April 19 to 27 - After a few bouts of dizziness and nausea that would come and go, Mom and Dad checked the Internet, checked Dad against a list of stroke symptoms they found, and then concluded that he must have an inner ear issue. But then he began having a few vision and hearing oddities, so they finally went to a clinic despite their nervousness about COVID-19 (at this point, they had already been homebound for several weeks).
April 27 to 29 - Dad was transferred to an area San Antonio hospital for 2 days of tests and observations. An MRI showed that he had experienced a TIA (Transient Ischemic Attack) or "mini-stroke", which surprised Mom and Dad, since he'd had no physical or mental effects that would signal a stroke. In fact, he continued to walk around and have calls with friends and business colleagues during those days at home and then during his time in the hospital as they tried, unsuccessfully, to determine the cause of his TIA. We heard later that he was hardly ever in his hospital room, and that the doctors and staff really enjoyed him at the hospital…Dad has a sharp wit and is a funny guy!
April 29, 2020 - On Dad's last planned night in the hospital, he had a massive stroke in the area of the brainstem that controls, among other things, involuntary (survival) functions of the body---breathing, swallowing, heartbeat, etc. They intubated him and put him on a ventilator. We were shocked, as were the doctors and nurses that had seen him so active and engaging during his time there.
April 30 - May 1 - Dad's doctors and caregivers must have realized that Dad was "in there" because they diagnosed him with Locked-In Syndrome, a rare condition in which he is fully aware, with full cognitive functions, memories, etc., but is paralyzed, unable to speak or move (with the exception of vertical eye movements). We were horrified upon learning about it.
April 30 - May 6 - During this first week, Mom and our brother Stephen, who also lives in San Antonio, received special permission from the hospital to visit him in the ICU, where he was sedated and on a ventilator. The hospital was NOT allowing visitors due to the COVID-19 pandemic and we learned later that they only gave permission because they thought he wouldn't survive.
This first week, we were asked to make a heartbreaking decision...either take him off of life support, in hospice care, sedated, and unaware of what had happened, or do two surgical procedures to give him more time: a tracheostomy (breathing tube in his throat) and a PEG (Percutaneous Endoscopic Gastrostomy) feeding tube. We knew that he had told Mom multiple times that he didn't want to be on a feeding tube, like his Grandmother, but we didn't know if he'd feel the same now. Bringing him out of sedation to make his own decision was a good idea, but that would also make him more aware of his situation and the doctors' prognoses were dire. They warned us that giving him more time didn't mean he would recover. Many people die because they don't come off ventilator successfully, or they have complications like blood clots, pneumonia from lying in bed. We were also on a heartbreaking rollercoaster ride with a variety of his doctors (many recommending the hospice route)---first we go up, with good news from his respiratory doctor that Dad was "over-breathing" the respirator (doing some breathing himself)---yay, Dad!---then the next day, we go down, with a palliative care doctor telling us about end-of-life options---boo!-- We were crushed.
May 6 - 8 - On the afternoon of May 6, Dad was brought out of sedation enough so that a doctor could tell him his prognosis and allow him to make the decision himself. Multiple doctors visited him over the next day or two to explain what had happened to him, to give him their perspectives, and to have him repeat his yes/no answer. Mom and Stephen also visited to ask him questions to test his memory and cognitive skills and to make sure he knew that we were with him no matter what! Each and every time, Dad chose to have the two procedures and take on the challenge! That’s our Dad! He is a fighter and we are so proud!!!
May 12 to 13 - Dad had the trach and PEG procedures performed and sailed through post-op recovery.
May 21 - Dad was discharged and transferred to Post-Acute Medical ("PAM") specialty hospital in New Braunfels for the next step in his recovery.
Dad's Ongoing Recovery (and Insurance Battles)
May 21 - June 24 - Dad was at PAM---a small hospital w a focus on respiratory issues and weaning patients off of ventilators. During these 6 weeks, he not only came off of the ventilator (achieved by only 50% of locked-in patients), but also twice had his trach tube reduced in diameter with no issues. This was a great success! Either Mom or Stephen could visit him EVERY DAY to give him love and support, bring him our audio and video messages, read to him, and hold his hand.
June 21 - with COVID-19 numbers rising over the previous weeks in Texas, due to its early open in May, the governor had to re-lock down healthcare facilities, and Mom could no longer visit Dad at PAM. This new lock down was especially difficult because we were told that Dad needed a new facility to move to by the end of that week. This meant we had to find a new facility for him, all without the ability to tour potential sites or meet with them in person!! All we could do was Internet research and phone interviews and hope for the best!
June 25 - Dad was moved to a Skilled Nursing Facility (SNF) for skilled nursing (trach, PEG and catheter) and rehabilitation services. The first two weeks were hard because the facility didn't have all of the equipment he needed and Mom couldn't visit him...all she could do is speak with people over the phone to check on him and tell people about his special condition and his equipment needs. Key people responsible for his care wanted to write him off and she had to tell them that "he is in there", what Locked-In Syndrome is, and what it means for his care. These early conversations and equipment delays did NOT help us believe that we had made the right decision!
July 6 - Finally, Mom could visit Dad, after getting a negative COVID test. She helped inform his caregivers and showed him our videos and encouraging messages.
July 14 - On this Tuesday, she came for a second visit and noticed that they finally had a good set-up in his room! She was approved for Tuesday/Friday visits and we were thankful that she could go 2x per week to check on him, participate in his care, and support him. All of his therapists told her that he was much more alert and focused when she was there and concluded that her visits are critical. By now, Dad's progress included moving his fingers in Mom's hand and working with his therapist to move his eyes laterally, instead of just up and down. Enter Dad's insurance providers, to "take care of" (destroy) all of those good feelings...
July 16 - After ONLY THREE WEEKS of skilled nursing and rehab at this facility, Dad's insurance providers, UnitedHealthcare and WellMed, handed down a decision to DISCHARGE Dad from care as of Monday, July 20 (even though he would only be in day 25 of the 100 days of skilled nursing and rehabilitation that is in his freaking policy)! Mom had until 12:00 pm noon on Saturday, July 18, to appeal this shocking decision. Mom wrote a long, handwritten statement and faxed it to the QIO, Quality Improvement Organization, a special 3rd party org that handles appeals. Over the next several days, Mom had to do this same appeal process two additional times (as did the QIO) because the facility didn't submit their clinical records to the QIO in time. Grrrr...
July 24 - Third time lucky! Dad's facility must have submitted their paperwork this time because Mom learned that the QIO had approved our appeal, determining that Dad's skilled nursing and rehabilitation were necessary. Such great news! Meanwhile, Dad had more improvements, like successfully moving his eyes from side to side. He is now ready to use a letter board to spell out words, instead of just answering yes/no questions with up/down eye movements. Yay! Mom also noticed him beginning to move his lips, tongue, and even swallow. This could mean that he may soon be ready to relearn his mouth control for breathing and swallowing, enabling future removal of the trach and PEG. He also "grasped" her hand multiple times, lightly bringing fingers and thumb together.
July 30 - Only 6 days after Dad's care is deemed necessary, ANOTHER DISCHARGE ATTEMPT is filed and needs to be appealed. Didn't we just do this??! Will we have to do this every 6 days? Really?? Mom had until noon THE NEXT DAY to fax in another statement. Since it'd only been 6 days, she faxed in the same statement. In the meantime, The facility is supposed to send in their clinical records. Hopefully, they remember to do this because Mom is spending $$ to send faxes from the UPS Store (they have no home phone). Four faxes so far!
August 1 - Appeal is DENIED because he hasn't shown enough progress. What? This past week, Dad has spelled several words on the letter board, has tracked with his eyes, has moved his head sideways, and has even held up his own head. HOW IS THAT NOT PROGRESS?? We are told to write a "Family Letter of Concern" and fax it in for "reconsideration" of the denial. We also got letters from his rehabilitation therapists for PT, OT, and ST stating that Dad needs their services, as well as skilled nursing, and sent it all on Sunday night, August 2nd.
And, now, we wait...(any later updates will be entered in "Updates" section)
We will continue to fight for Dad to not only receive his full 100 days of benefits (which are abysmal anyway, compared to the many months to a year of rehabilitation therapy that he will probably need), but also to receive some CONTINUITY of care, with a group of therapists and nurses that he knows and trusts! He can’t keep moving from site to site every few weeks, as soon as we have a great team of caregivers working with Dad and fighting alongside him.
Please pray for our Dad!
Locked-In Syndrome – What Is It Like?
Locked-In Syndrome (LIS) is a rare condition that few seem to understand in the medical community. At first, most locked-in people are thought to be in a vegetative state, since they are motionless and have to be put on life support systems, like ventilators and feeding tubes. Later, someone---many times, a family member, but it can also be a doctor or caregiver---recognizes that the patient is present and aware, which leads to an LIS diagnosis.
There are several articles, books, and videos out there that tell the story of what it is like to be locked in. These people are at varying points in their recovery from LIS and have different ways of communicating---blinking, letterboards, or speaking---but all have been able to tell their story in their own words:
1. Voicing Inner Thoughts Matters | TEDx - Talk given by Kate Allatt, who had a brainstem stroke and LIS, started the site fightingstrokes.org, and wrote 3 books.
2. Breaking out of Locked In Syndrome with Richard Marsh - an article about a retired California police officer who suffered a brainstem stroke and LIS. See an interview of him here on YouTube . He also wrote a book called Locked In: One Man's Miraculous Escape from the Terrifying Confines of Locked In Syndrome.
2. How My Mind Came Back to Life and No One Knew | TEDx - Talk delivered by Martin Pistorius using speech synthesis, a form of Augmentative and Alternative Communication. Martin suffered a childhood illness at 12 that devolved into Locked-In Syndrome. He has also written a book called Ghost Boy.
3. The Diving Bell and the Butterfly - a best-selling book by Jean-Dominique Bauby, Editor-in-Chief of Elle Magazine who suffered a stroke and LIS in 1995; the book was made into an award-winning movie of the same name in 2007.
4. The Patient's Journey: Living with Locked In Syndrome - an article on the National Institute of Health (NIH) website from the point of view of Nick Chisholm, who suffered a traumatic injury during a rugby game which led to stroke and LIS.
#LockedIn #Locked-In #LockedInSyndrome #Locked-InSyndrome #Help #StrokeSurvivor #TBI #BrainInjury #Stroke #StrokeRehabilitation #StrokeEducation #StrokeAwareness #Health #TeamDon #FightForTeamDon #Fight4TeamDon #Don'sVoice #DonsVoice #Veteran #Marine #Health #Recovery #Rehab #NeverGiveUp #StillMe #Neurorehabilitation #BrainStem #Paralysis #Aphasia #Disability #Physiotherapy #SpeechTherapy #Neurology
 Fundraising team: Williams Family Team4
Fundraising team: Williams Family Team4
Sue Williams
Beneficiary