Justice for Jeannie
Donation protected
My name is Babbette Kurtz. I'm fundraising to help bring to justice the medical professionals responsible for the heartbreaking agony and death of a beloved and talented colleague and one of the best friends I ever had.
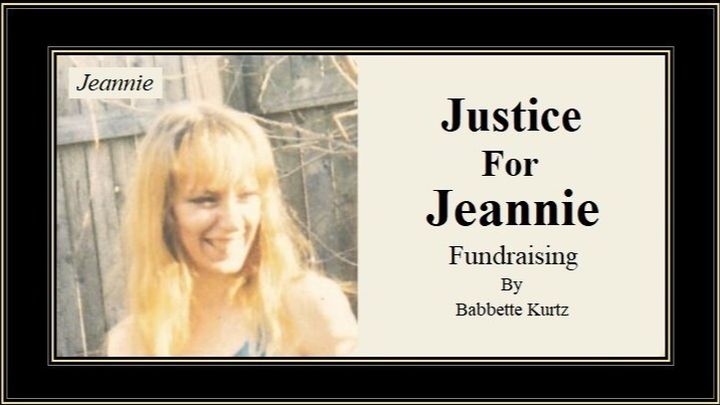
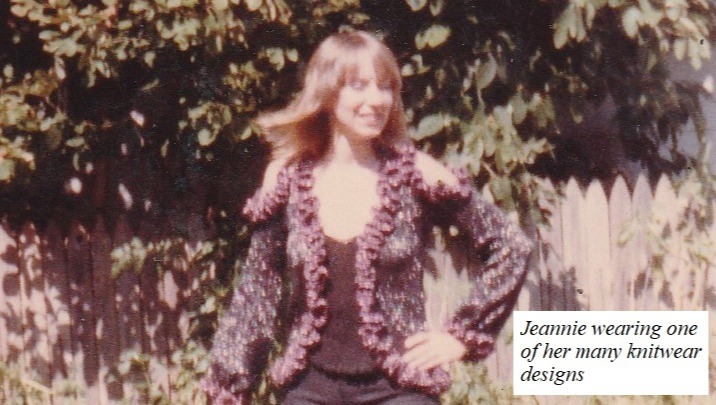
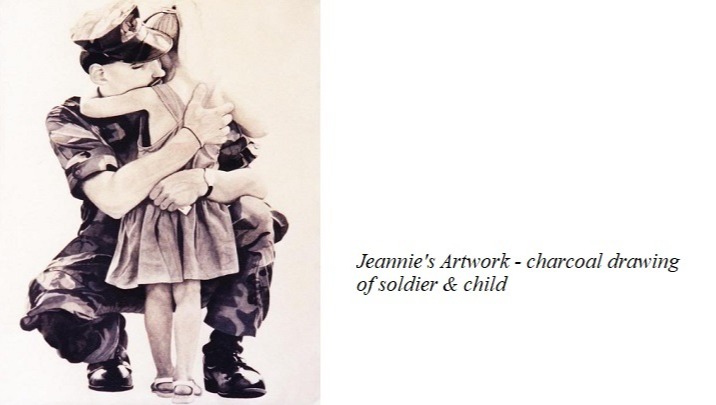
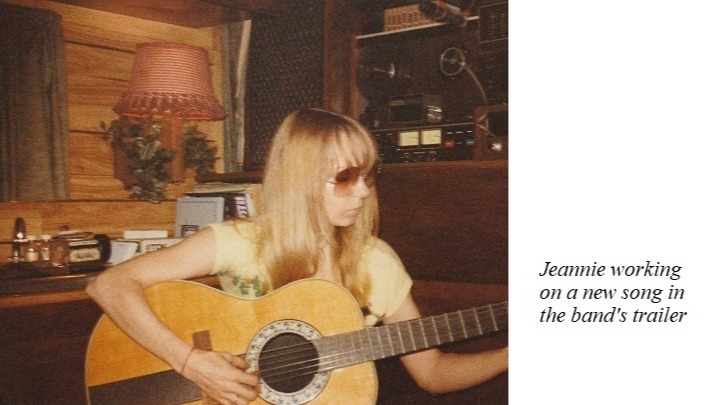
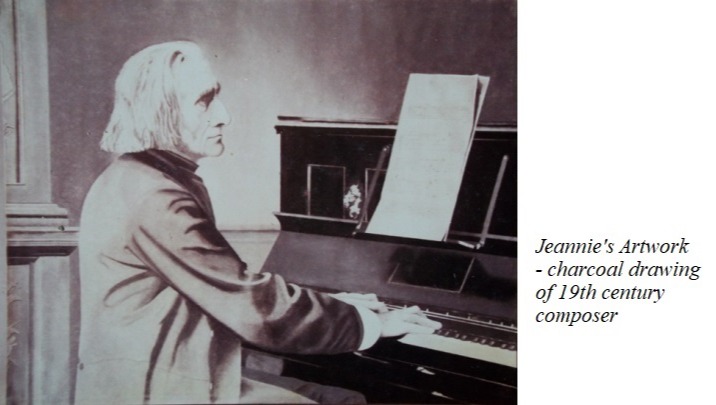
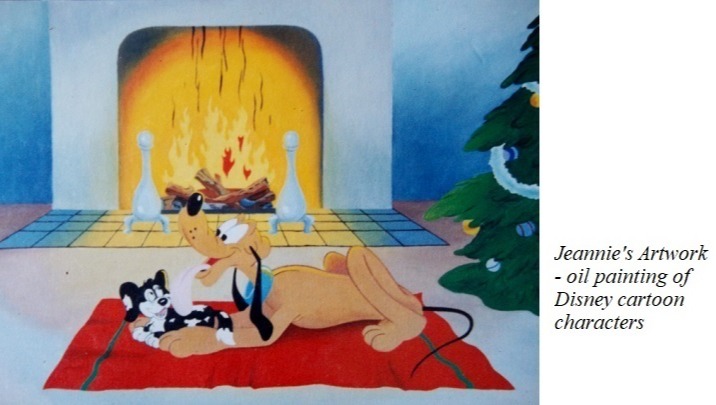
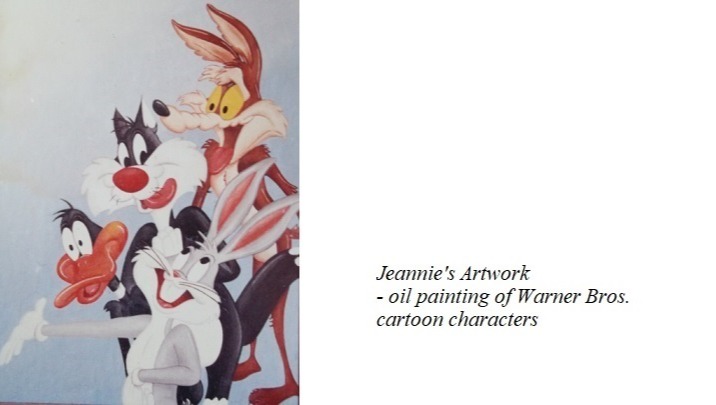
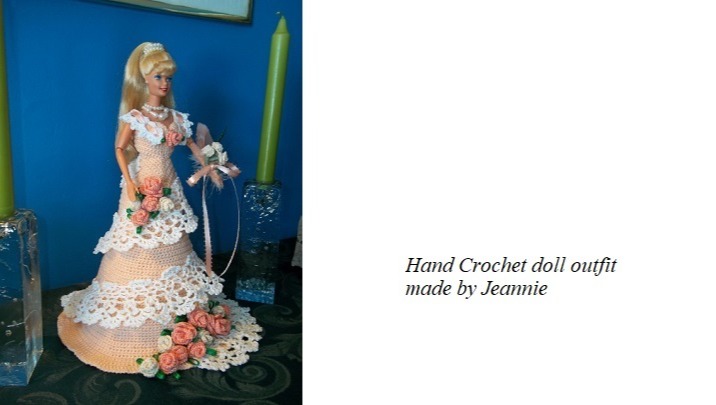
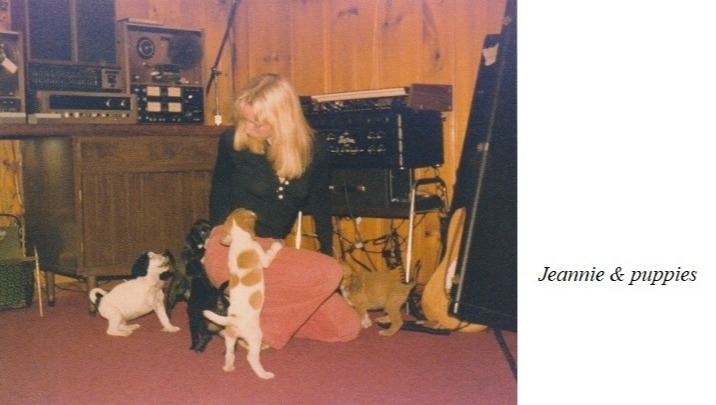
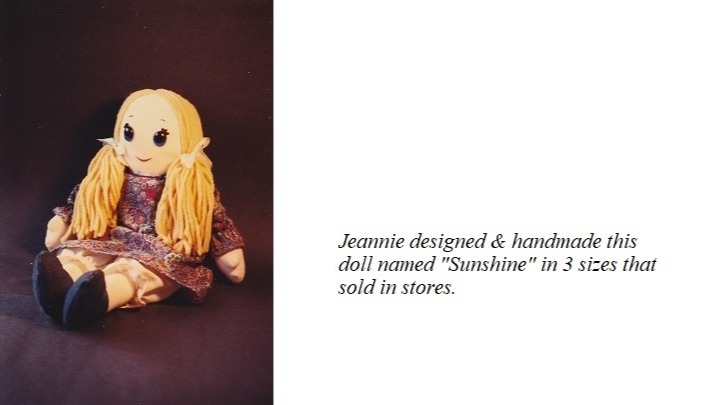
I was 15 years old when I first met Jeannie Christiansen. She was in her early 20's. Jeannie had pretty blue eyes, long blonde hair and an endearing smile. At the time, she was making clothing, dolls and ornaments that she could sell in stores and boutiques. She had been together with Mike Charla for almost 5 years. They seemed perfect for each other. Both were musicians, artists, writers, hot rod enthusiasts and animal lovers.

As the years flew by, we all remained good friends and even began to play and record music together. It was like having our own personal soundtrack. At the same time, Jeannie had been making a name for herself in the fashion industry, designing and machine knitting high fashion garments for several fashion labels across the country. And she was great at it, eventually employing over a dozen people on a steady basis.
But, the fashion industry is fast-paced with tight deadlines. And I won't even attempt to characterize the music business. When they had to move Mike's disabled mom into the house, the daily challenges only increased. Jeannie never thought of herself as being 'stressed out', but her doctor thought a Xanax script might benefit her anyway.
For those who don't know much about it, Xanax is considered a controlled substance that treats anxiety and panic attacks. Since the early 1980s, it was the drug of choice to treat these disorders and many doctors still prescribe it today. If discontinued, it must be tapered off gradually and closely monitored. Jeannie took Xanax for 6 years with no side effects. She was happy, healthy, and doing all the things she loved.
When Jeannie's doctor left his practice, he referred all of his patients to other medical facilities. Upon taking over her case, the new doctor failed to renew Jeannie's Xanax script for almost 2 weeks, causing her to have seizures for the first time in her life. A second doctor at the same facility would only prescribe anti-depressants, which didn't agree with her. He told her to go to an emergency room if she wanted Xanax. But every E.R. within 2 counties told her to go back and get it from her doctor. Now increasingly fearful of more seizures, Jeannie was suddenly being treated like an outcast begging for loose change.
While Mike relentlessly searched for a new doctor, he was consistently running into one major obstacle. Not all doctors were still prescribing Xanax. The excuses varied. To name a few, there were the highly debatable claims of addiction, unrealistic fears that teenagers might sell it on the street corner (there were no teenagers in Jeannie's household), and scantily researched claims of "possible" memory problems 20 years down the road. There was just one glaring omission in Big Pharma's list of excuses: Xanax could be purchased for 1/10th the cost of the "new", far less effective, anti-depressants that so many doctors were now pushing on their patients. Further research turns out that there are internet forums flooded with people seeking Xanax because their doctors cut them off.
The psychological injuries Jeannie sustained as a result of her Xanax being cut off included: shaking, severe chronic anxiety, acute panic attacks, seizures, memory loss, and PTSD. The physical injuries she suffered included: falling down a flight of stairs, smashing her head on a porcelain bathtub, falling down unconscious on cement, in a store, in the street, and even out of her own bed. All taking place amid multiple 911 calls and nerve-racking trips to emergency rooms.
Another medical facility would only prescribe a fraction of the 3mg daily dosage Jeannie required. Her seizures continued. Mike suffered what he later learned was his first heart attack in the examination room with Jeannie while trying to convince the NP in charge to prescribe the Xanax dosage proven to be effective in the past. Begrudgingly, the NP finally complied. But 3 months later when the NP took an extended medical leave and was replaced by a staff psychiatrist, he immediately cut Jeannie off again.
Nearly frantic at this point, Jeannie went to see Mike's doctor, who they already knew was against prescribing Xanax. By sheer luck, she was instead seen by a sympathetic NP who worked there. After hearing what Jeannie had been through, she prescribed the original script that worked flawlessly for 6 years.

For the next three months, Jeannie focused on regaining the strength and mobility she had lost. Even her PTSD, the result of doctors wreaking havoc on her mind and body, was beginning to subside. Her hands still shook and she still wouldn't attempt to drive, but at least she began using stairs again. For the first time since the whole awful ordeal began, there seemed to be light at the end of the tunnel.
But, midway into the fourth month of her convalescence, Jeannie noticed something that didn't make sense. The dosage and instructions on her monthly Xanax script were correct (1mg 3x a day), but the vial only contained 60 pills rather than the usual 90. She was going to run out. The NP who wrote the prescription gave no tangible medical reason for the sudden decrease or the misleading instructions but did offer a vague recitation online regarding nonspecific rules and laws. This was the first time Jeannie was hearing about any of this. Her best efforts to stretch out what was left of the pills could not stop what soon followed: a rapid onset of seizures, a stroke and cardiac arrest.
Mike was with her when it all happened at once. Jeannie wasn't breathing and he couldn't detect a heartbeat. He immediately called 911 and began CPR, twice reviving her before the medics arrived. In the emergency room, Jeannie's heart stopped again, leaving her on life support, fully sedated, and in "very" critical condition for 20 days.
Without delay, Mike moved into Jeannie's hospital room in the intensive care ward and stayed with her day and night until she was able to come home.
After being discharged from the hospital, Jeannie's follow up care included seeing a heart specialist. Mike brought her to the cardiologist he had started seeing after his own heart attack. Since Jeannie no longer had a personal care physician she could trust, she was concerned about the possibility of needing Xanax again. The cardiologist said he could not prescribe it himself, but referred her to a doctor who he knew personally.
When Jeannie's medical records were transferred to the new doctor, she was told that they wouldn't accept patients who abused their medication with alcohol. Something Jeannie had never done. But when she obtained a copy of her medical records for herself, they painted a very different picture.

In the past, when Jeannie's Xanax script was suddenly cut off, a shot of vodka every four hours helped to reduce her anxiety symptoms. She would sometimes alternate the vodka with Benadryl (Jeannie wasn't a drinker). Her last doctors, who she had made aware of this, falsely claimed it to be "drug and alcohol abuse" in her medical records. It was not written out in English, but in medical code that Mike had to look up.
Upon learning of this abject lie on top of all Jeannie had already been through, she and Mike spoke to a number of attorneys who all said that because there were several doctors implicated, legal action would involve complex litigation and that they were reluctant or weren't equipped to take on multiple medical facilities simultaneously.
To avoid being barred from filing suit due to the statute of limitations, Mike proceeded pro se (without a lawyer), a nearly impossible task given the complexity of the actions, not to mention the fact that he's not an attorney.
Meanwhile, they were having no luck finding a doctor within a hundred-mile radius who was taking on new patients and still prescribing Xanax. And then there were the false statements in Jeannie's medical records to be concerned with. The general consensus in the online forums was to not ask for Xanax upfront. But Jeannie didn't have time for that. Her panic attacks and PTSD episodes were becoming more frequent and severe again.
It was a sunny April morning when Jeannie died of cardiac arrest. She was laying on her bed when Mike found her. Just forty minutes earlier she had smiled at him when he brought her breakfast. As an avalanche of thoughts coursed through his mind, Mike called 911 and began CPR. But this time, nothing anyone did could bring Jeannie back.
As time inched forward and the outside world crept back into focus, Mike knew that Jeannie wouldn't have wanted him to remain steeped in futile legal battles with high-powered attorneys. But would she want the negligence, incompetence, and blatant wrongdoing that caused her suffering and death to go completely unaccounted for? And if nothing were done, how many others would suffer a similar fate?
The legal actions that Jeannie and Mike initiated can still be salvaged, but they are very costly and won't be sustainable for much longer. A competent attorney who specializes in medical malpractice and wrongful death is vitally needed at this point.
Jeannie was the kindest, sweetest person I've ever known. She brightened every room she entered and had so much more life to live. A life that was tossed away by a broken healthcare system that allows self-serving doctors to play God with complete impunity the moment the examination room door closes.
Any effort to stop unethical practices by medical professionals can make a difference for many. Especially if the problem is systemic. This, through tremendous struggle and grievous loss, is one of those efforts.
The legal actions are of public record. All funds go directly to the beneficiary. Any help you can offer would be thoroughly utilized with heartfelt gratitude.
Please share this link.
Organizer and beneficiary
Babbette Kurtz
Organizer
Phoenix, NY
Michael Charla
Beneficiary