Thankyou all, from the bottom of my heart for all of your thoughts, prayers, concerns, confidence building advice, encouragement, and inspiration…and, to Grandma Rose and my mom, and Grandpa George and Grandma Matie for being our foundation of consistently virtuous behavior by your teaching and most importantly your role modeling.
Here is why: On June 7th, 2016 I was driving down Lamb Blvd. in Las Vegas, NV heading toward Charleston Blvd., so I could merge onto I-95 North; then to the spaghetti bowl which would take me I-15 South to the Mandalay Bay.
I was close to Charleston Blvd. with my right blinker on waiting to merge into the right turn lane when a car cut me off, and slammed on their brakes. I attempted to miss them, but they had used up any safety margin I'd created which left me no safe option, so I in turn slammed on my brakes and hit them. The impact threw me forward and diagonally to my right where I hit the windshield with my head, and shattered it. The impact with the windshield also opened a three inch cut in my scalp which bled down my face, and onto my white shirt. The force of the impact threw me violently back into the driver's seat, and hurt my neck and shoulders.
The first thought that came to me was that I had better shut off my vehicle in case there was a gas leak, and a possible explosion. I then put my car in park, and turned on my flashers. I then thought that I should get out of my vehicle to check my flashers to make sure they worked, so no one would rear end me. I in a stupor I continued to walk around the back of my vehicle and to the vehicle in front of me to check on them.
As I was walking back to my vehicle to sit down in case I passed out two paramedics/firemen were running toward me. Probably the blood over my face, hair and white shirt were alarming them. They asked me to sit on their stretcher and they started to assess me: When they asked me my name, I responded, but I slurred my speech so badly they asked me if I had been drinking. It was six-thirty in the morning! And, I don't drink! He then asked me to hold his hands and squeeze them. I am generally pretty strong, especially in my left hand because I'm left handed, but I could hardly squeeze his hands. He then put his hand by the left side of my head, and asked me how many fingers he was holding up. I could not only tell how many fingers he was holding up. I couldn't clearly see his hand! I was rapidly losing my peripheral vision! He then expressed that the left side of my face was sagging.
He knew I was in serious trouble, so he asked me which hospital I wanted to go to. I told him Sunrise Hospital because I had heard from a colleague they had a good head trauma unit.
They took me in their fire truck/ ambulance to Sunrise Hospital (Which I don't remember.). The paramedic called ahead to let the personnel at Sunrise Hospital know that I was coming, so they could be ready. When I arrived a neurosurgeon, Dr. Lin, and a neurologist were waiting for me in the emergency room.
They put me on a CT scan which showed I had a blood clot in the right, rear hemisphere of my brain. Specifically, in my M2 artery. They explained to me that they couldn't give me clot busting drugs because it could cause hemorrhaging in my brain because of the severe head trauma. The only option left was a thrombectomy procedure (click here to view a YouTube video of the procedure). This procedure involved making an incision in my groin into my femoral artery, and inserting an instrument with a camera and a device to remove the clot into my femoral artery and pushing it through the artery up into my brain until they could find the blood clot and remove it. They asked me to sign some papers prior to performing this procedure. Here I am lying on my back on a stretcher, bloody, a long gash in my head, thinking I've never been in hospital, let alone know if a thrombectomy procedure is safe. I mean you're going to go into my brain with this thing! Geez! So, I said to the neurosurgeon, Dr. Lin, may I borrow your phone, so I can call my sister, Kim, who is a RN, so I can ask her if I should do this? He handed me his phone and as I was laying on a stretcher, bloody, experiencing various symptoms’ of a stroke I dialed Kim and expressed to her, "Kim, I'm in the emergency room at Sunrise Hospital in Las Vegas with a blood clot in my brain. The neurosurgeon, Dr. Lin, and the neurologist, Dr. DeAndrea want to perform a thrombectomy on me to remove the blood clot. Should I do this? Is it safe? Please call me back." I hung up the phone, and gave it back to Dr. Lin. I told him I couldn't get any feedback from someone I know and trusted, that is, my sister, Kim, so I momentarily lay there. Without skipping a beat Dr. DeAndrea, said, "If it were me I'd do it." He said that with such a calming, and trust engendering effect on me that I felt secure in signing the paper (I'm sure he was thinking something to the effect, "Seconds lost, is brain lost.). With that, I signed the paper for Dr. Lin to do the thrombectomy. They anesthetized me, and opened up my femoral artery in my groin area, so he could maneuver the device with the camera on it that would remove the blood clot. (Oh, somewhere in between entering the emergency room and now I remember someone talking to me and rummaging through my hair tracing the bleeding. They found the gash in my head and stapled it shut.) What seemed to me to be in a short time I remember Dr. Lin exclaiming, "I got it!" There was celebrating (As best I can remember being prone, and anesthetized.).
I then was moved to intensive care in the Neurosciences section of the hospital for observation, testing to attempt to determine where the blood clot came from in the first place with the intent to avoid a second stroke.
An IV was inserted into my left arm (another first for me...) which stayed there for nine days.
I basically rested for the rest of the day which was interrupted by blood tests, IV bag changes, blood pressure readings, blood draws and so forth. I was pretty much in a state of shock that all the above had happened to me, and wondering on some level if things were going to be 0.K.. I recall thinking that I had not smoked or done drugs or drank to avoid things like the above. So, I kept wondering what I had missed or what didn't I know that I should have done? Nothing was coming to me...so I just tried to relax.
I called my sisters, brother, cousins, aunts and uncle and mom.
Kim, who I had attempted to reach prior to the thrombectomy, called me back to let me know that she had got my message, and the message sounded like I was "drunk". I still was unaware of how I sounded, but I know Kim wouldn't misrepresent the way I sounded (She saved the answering machine message for evidence.). Eventually, I laughed about it, but it still is disconcerting to me that one can basically "feel" fine while simultaneously having part of your brain be in the process of dying. Maybe I still will have this disconnect forever because my only (or anyone's for that matter...) reference point - my brain - wasn't functioning well, so I couldn't cognitively appreciate that my face was drooping (left side), my speech was slurred, my peripheral vision on the left side of my head had deteriorated rapidly, and I virtually had no grip strength in my left hand and so forth.
Kim told me that Chris and she were going to fly out tomorrow, the 8th. I told her that I appreciated that, but on some level I didn't want to disrupt their work schedules, and that I felt fine. She exclaimed, "Brian, you just had a stroke!" With that, my stroke effected brain was looking forward to them being with me on Wednesday.
Kim and Chris, arrived at about 11:00 a.m. on the 8th. Dr. Zafar, my cardiologist, had done some testing on my heart on Tuesday, but didn't find evidence of any blood clots. He wanted to do another test on my heart called a Trans esophageal echocardiogram (click on Trans esophageal echocardiogram to see a YouTube video of this procedure) to look at the back side of my heart for any evidence of blood clots. Eventually, it was scheduled for Thursday, the 9th of June.
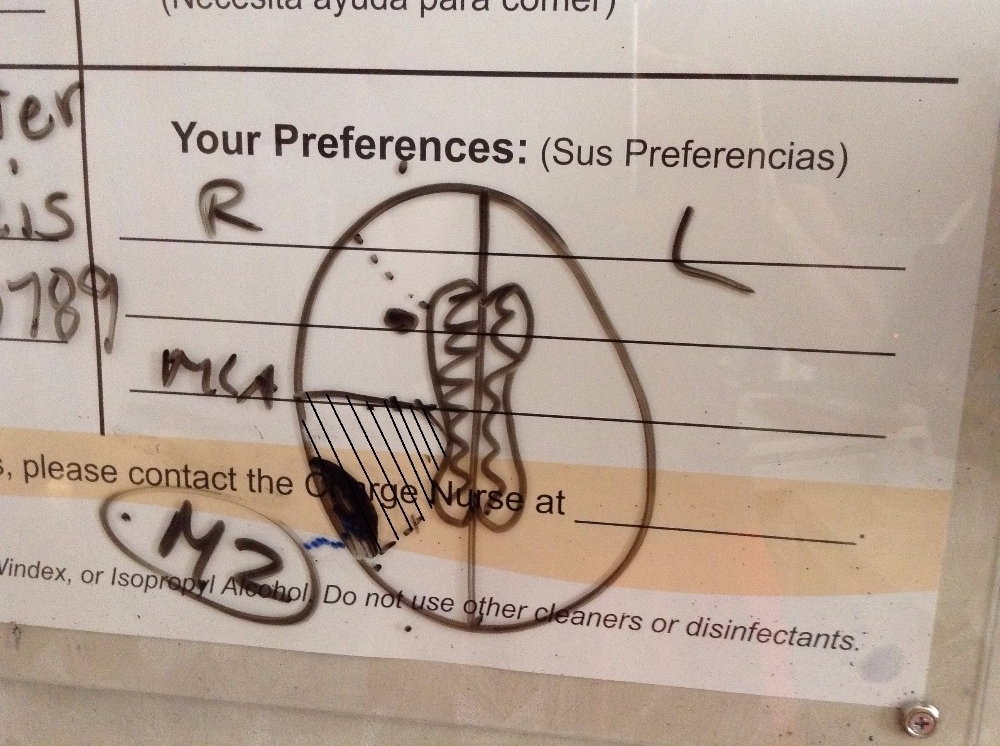
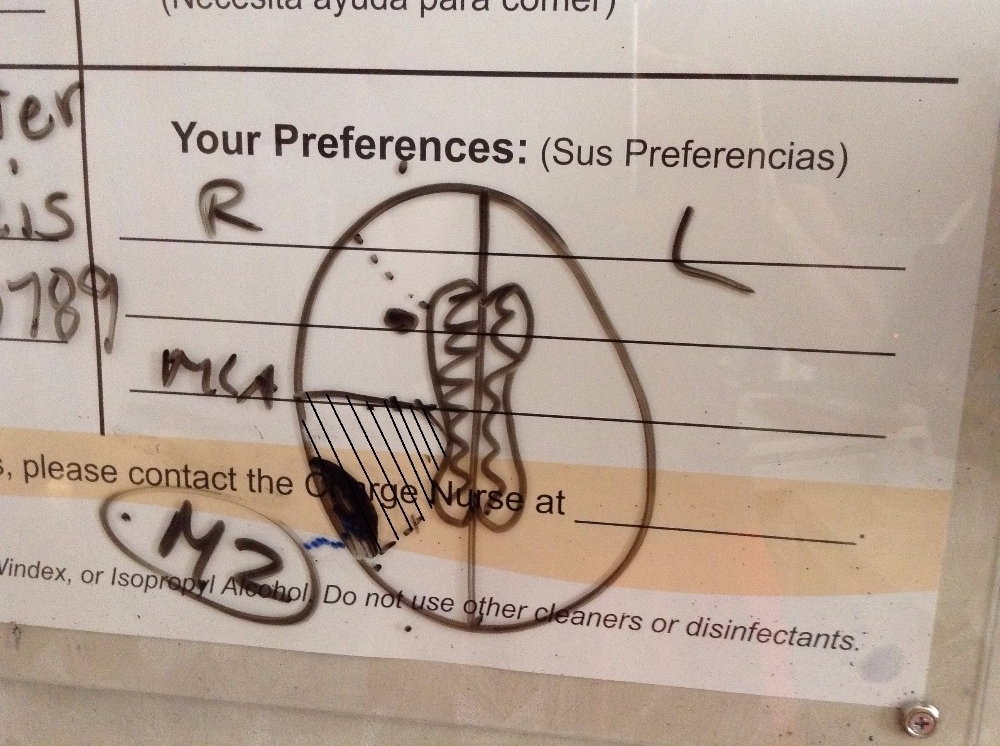
On Wednesday, June 8th, prior to Kim and Chris arriving at around five-thirty in the morning I was transported to have a MRI. That showed the area of my brain that was effected by the stroke which was minimal compared to the size of my brain tissue that would have been destroyed had Dr. Lin not removed the blood clot from my M2 artery. Because of the paramedic/fireman's training in recognizing symptoms of a stroke and his speed in getting me to the hospital, Dr. Lin’s and Dr. DeAndrea’s expertise in advising me and their skill in brain, blood clot removal I avoided being paralyzed on the left side of my body or dead. Dr. DeAndrea drew a picture of the area that would have been lost of the right hemisphere of my brain, if the blot clot had not been removed (Reference the cross-hatched area in the picture taken by Kim, below) and ,also, he drew a dark spot on my brain that the stroke had effected (Reference the dark spot adjacent to the cross-hatched area in the picture taken by Kim, below.). That dark spot represents, minimally, sixty million brain cells. A person loses approximately one million brain cells per minute while having a blood clot in their brain, which is a stroke.
Kim and Chris had to leave to go back to the airport prior to my completing the Trans esophageal echocardiogram, but as I was recovering from the procedure in the "Cath Lab” Dr. Zafar briefed Kim and Chris on what he had found. The good news: He didn’t find any evidence of any blood clots in the back side of my heart! The mixed blessing news: He found that I had a hole in my heart between my atriums (the upper chambers of my heart, and yours, too.). I'm not sure if Dr. Zafar had explained this to Chris and Kim prior to them having to leave for Des Moines, but I learned from him and others after being transported back to Neurosciences Intensive Care from the "Cath Lab” that a hole between the atriums can slow the blood flowing from the left atrium(deoxygenated blood)into the left ventricle sufficiently that a blood can form a clot which may migrate to the right atrium, and, consequently, be pumped into a person's brain(in this case that person may have been me, but because there isn't presently available instantaneous testing that can conclusively show this no one will ever know for sure, but it is reasonable to deduce that in my case that this probably was the case.). For all of you NFL fans and particularly New England Patriot fans approx. a decade ago Tedy Brushi, a linebacker for the Patriots and a University of Arizona graduate, had a stroke a couple of weeks after his third Super Bowl appearance, and after diagnosis and testing at Mass. General, the doctors there discovered that he, too, had a hole in his heart, but in Mr. Bruschi's case, his was between his ventricles or the lower chambers of his heart. Mr. Bruschi does an excellent job of detailing his experiences- his fight- through this process in his book: Never Give Up: My Stroke, My Recovery, and My Return to the NFL.
This news from Dr. Zafar was at the very, very least disconcerting. I had never heard of a PFO procedure , (click on PFO procedure to see a YouTube video of the procedure) just like I had never heard of a thrombectomy.
I wasn't really sure where to begin in deciding to have the PFO procedure or not. I knew everything in my being wasn't ready yet.
But somewhere along the line someone scheduled me for the PFO procedure on Friday, the 10th of June, 2016 @ 4:30 p.m... I was trying to get myself psyched up to do this, but I was to conflicted/unsure to proceed so, I called Ticey, my nurse practitioner. She came to my room and we talked about the pros and cons of this procedure. Using a blood thinner to cope with possible future blood clots, etc.. Even though Ticey did an excellent job of trying to help me sort through my concerns I just couldn't come to a decision that I was comfortable with, so I told Ticey I needed more time. She asked me, "How long would you like?" I said, "A couple of days to do research."
I started by calling Aunt Gretta who was a surgical nurse. She in no uncertain terms stressed that the cardiologist who would perform the procedure had to have performed it many times.
That was the first priority in selecting a cardiologist: A lot of experience with this specific procedure.
I then called my first roommate at Iowa State University who is a pathologist and a Professor of Medicine at The University of Chicago. Tony asked other doctors at the University of Chicago who had experience/ knowledge in PFO procedures. Tony called me back and told me that his colleagues had done many of these procedures, and usually, the only time doctors discover that someone even had this done is when they do an autopsy. He assured me it was safe, and that the procedure had been around awhile. Those affirmations, along with my sister, Kim, and my brother-in-law, Dennis, gave me confidence I should proceed with the procedure even though I had some reservations that were referenced in the neurology literature versus the cardiology literature. I called Stanford University, The Cleveland Clinic, Loma Linda University and others to try to more thoroughly understand the risks, if any, with the procedure, the long term consequences, while following-up on Aunt Gretta’s advice to find a cardiologist with a lot of experience in this specific procedure. The drawback with going out of state was the continual follow-up appointments in cardiology, neurology, my general practitioner, etc....
After a lengthy search from my hospital bed, a good friend of mine, Marv, called me to let me know that a close friend of his who was a Yale Medical School graduate, and a thoracic surgeon recommended Dr. Zafar. Because of my confidence that Marv was trustworthy I felt confident that staying in Las Vegas, and letting Dr. Zafar do the procedure was a wise option. That also took the burden off of me of the time and travel expenses with follow-up appointments at other out of state medical institutions.
So, with that, I had my immediate nurse call Ticey (my nurse practitioner) that I was ready to do the PFO procedure and have Dr. Zafar do it. Given I had no prior knowledge of a PFO procedure to help me make this decision I think I could have researched for the next two months and still not felt psychologically or emotionally comfortable with it. I do know one thing about it for sure: Chris, my sister, told me after the procedure that she had watched it on YouTube, and said something to the effect that, "I don't know if I'd do that!" Thank you, Chris, for your restraint by NOT telling me that until after I had gone thru the PFO procedure. I expressed that, like I said to Ticey on the 12th of June, 2016, but I don't recall anyone ever coming to my room to verify when it was going to happen on Monday, the 13th of June. I do remember that I couldn’t eat anything the night before, and until the procedure was done. I do remember that at roughly 4: 00 p.m. on the 13th two guys from the "Cath Lab"(Actually, the same two guys that had prepped me for the trans-esophageal echocardiogram.) came to my room to put me on a gurney and take me down to the "Cath Lab" to prepare me for the procedure. I still hadn't gotten a crystal clear idea of what was going to be done to me, so I asked them, and with the help of a video of the procedure while lying on the operating table I turned my head sideways to watch it while they did an excellent job of explaining. Shortly, after that, Dr. Zafar came in, cut into two of my veins in my groin and, first, inserted a camera into one vein to travel up to my heart, to determine the size of the hole between my atriums. The second incision in my groin was used to insert the correctly sized titanium device and guide it to my heart, insert it on either side of the hole between my left and right atriums, and, finally, to tighten it. When all that was done Dr. Zafar showed me the device in my heart on a jumbo size screen to my left. From my perspective it looked like two parallel wheels with a small space in between them. (Oh, I forgot to mention, one critical detail, that is, prior to inserting the camera or the properly sized titanium device between my atriums there had to be two roughly eight inch long and one-quarter inch in diameter plastic tubes (see picture, below.)
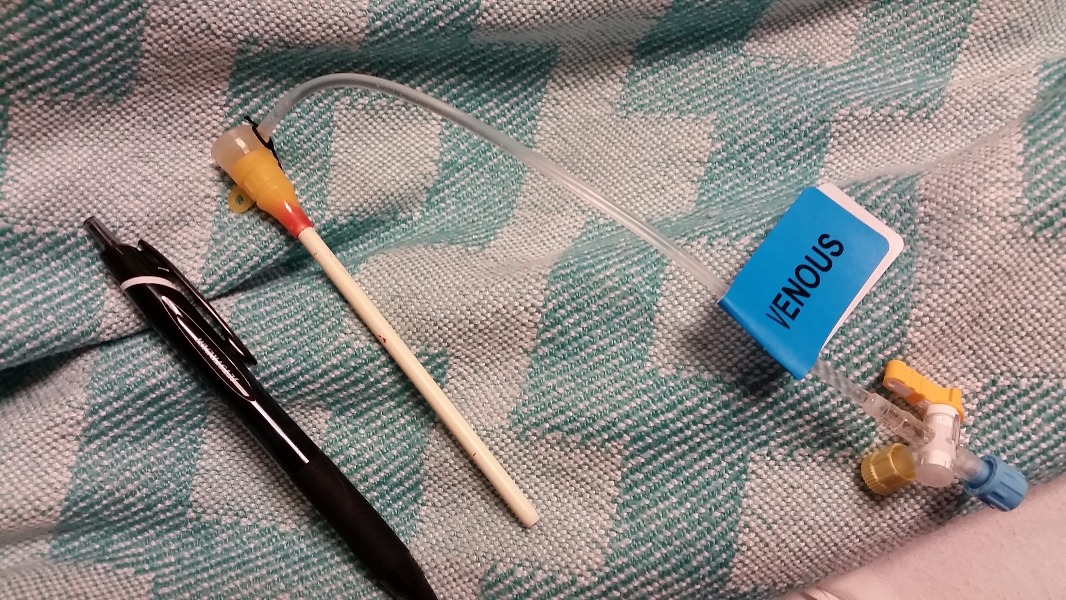
inserted in each vein to help them maintain structural rigidity enough to allow a camera or a titanium heart repair device to enter either vein.). After this I was moved from the very cold "Cath Lab” to the recovery room. Bruce, my recovery room nurse, gave me specific, very stern directions about what he and the other nurses were going to do, and what I needed to do, which was: A.) Bruce and the other nurses job: 1.) First pull out one of the plastic tubes from the vein in my groin very quickly while immediately placing heavy pressure on the incision area for twenty minutes, 2.) Then quickly pull out the other plastic tube from the other vein in my groin, and, again, place heavy pressure on it for twenty minutes, and, 3.) My part: DON'T MOVE! NOT EVEN A SMIDGEN for the next six hours! That included not lifting up my head even an inch (Or even less than an inch!)! Bruce made this unequivocally clear: If I'd move, and either or both of the incisions started to bleed the whole process would have to start again, that is, heavy pressure on each incision separately for twenty minutes each and starting the counting of the six hours from zero.
The thought of the strict tolerances for laying still, and the negative consequences, that is, twenty more minutes of pressure on each incision, and six hours of laying still was fear provoking enough not to think about it. But, trying not to think about it was a tough discipline for six hours. But, the thought of having to start all over again was worse, and sufficient motivation for me to apply extreme mental focus to lie still.
The next few days in the hospital were mostly spent walking with physical therapists, talking to a speech therapist, an occupational therapist, my internal medicine doctor, Dr. Syed, about blood thinners, etc., and I was released from the hospital on the 15th of June, 2016.
While in the hospital I told various people that my right shoulder hurt, but obviously heart and brain function took priority, so when I was trying to shower and get dressed (which I hadn’t done for nine days) I couldn’t use my right arm without severe pain. I attempted to work through that for days, but it continued to persist which brought me to the point of getting it x-rayed, and seeing my general practitioner, Dr. Miller, who referred me to an orthopedic surgeon.
I can’t have another MRI for six months because of the titanium device in my heart (The strong magnetism generated by an MRI machine can potentially dislodge the titanium device), so the orthopedic surgeon couldn’t order one of those. But, physical therapy, twice a week for the near future was prescribed. Determining positively whether or not I have a tear in a ligament, tendon and/or a muscle will have to be delayed until a more definitive diagnosis using an MRI can be done.
I will be undergoing more diagnostic measures, hopefully, in the near future to determine if I have a blood clot on the inside of my femoral artery, and/or my veins at the incision site(s) for the thrombectomy procedure and the PFO procedure. I’ve been experiencing sharp pain in this area, so it warranted being followed-up with.
Sixty-million dead brain cells had a significant function for me, but what? Even though an hour is considered a relatively quick response time for the removal of a brain, blood clot it still can cause abnormal brain function because of the sheer volumn of brain cells lost, so I am going to see a neuropsychologist for evaluation, and hopefully, establish a baseline of what psychological, emotional and physical deficits it caused, and what can be done to get those functions back to normal.
Today, 23 August, 2016 I received a new referral from my orthopedic surgeon to continue physical therapy because my shoulder is at about six percent of its normal strength. For example, I can curl only three pounds where prior to the accident I could curl fifty pounds or more.
An ophthalmologist will evaluate my peripheral vision to determine if it is sound, hopefully, in the near future. It continues to improve.
I am learning to be aware, and sensitive to what before I may have considered a small pain, and disregarded it. That learning process and follow-up will be ongoing for at least six months while I am on disability.
My immediate and long term goal is to take sound, baby steps forward. Be patient. Heal thoroughly, and build mental and physical strength gradually and prudently.
I do not have any definite timeline to be back to work, let alone any vigorous physical activity, but I am confident that Dr. Zafar, my cardiologist, Dr. DeAndre, my neurologist, Dr. Miller, my general practitioner, Tim Soder, my physical therapist and all my relatives pictured at the beginning of this (and the many more not pictured), and all my friends: Evonne and Larry, Lothar, Steven, Michael, Kathy, Karen and Erek, Stephan and Pat, Jerry, Rudy and Sabrina, and Katie C. will get me there safe and sound.
And, a uniquely, special thanks to Tedy Bruschi and his wife, Heidi, for your heartfelt care and concern and unselfish forsight to want to share the details of your stroke experience with the hope that it would provide encouragement, and hope for a full recovery to all those experiencing one. I asked Dr. Zafar at some point in this process, if he ever thought that I could run, again. The first thing out of his mouth was your name, that you had experienced a stroke and a PFO procedure, and had rehabilitated and returned to the NFL. The NFL has never been part of my job description, so returning to it won't be one of my goals, but running a roadrace like Falmouth, hopefully, someday will be.
Thankyou, infinitely, for and to the Creator of all life, Jesus of Nazareth for without Him even the possibility of generating thoughts, let alone thoughts about one of HIS creations, our brains, wouldn't exist.
Sincerely,
Brian
Here is why: On June 7th, 2016 I was driving down Lamb Blvd. in Las Vegas, NV heading toward Charleston Blvd., so I could merge onto I-95 North; then to the spaghetti bowl which would take me I-15 South to the Mandalay Bay.
I was close to Charleston Blvd. with my right blinker on waiting to merge into the right turn lane when a car cut me off, and slammed on their brakes. I attempted to miss them, but they had used up any safety margin I'd created which left me no safe option, so I in turn slammed on my brakes and hit them. The impact threw me forward and diagonally to my right where I hit the windshield with my head, and shattered it. The impact with the windshield also opened a three inch cut in my scalp which bled down my face, and onto my white shirt. The force of the impact threw me violently back into the driver's seat, and hurt my neck and shoulders.
The first thought that came to me was that I had better shut off my vehicle in case there was a gas leak, and a possible explosion. I then put my car in park, and turned on my flashers. I then thought that I should get out of my vehicle to check my flashers to make sure they worked, so no one would rear end me. I in a stupor I continued to walk around the back of my vehicle and to the vehicle in front of me to check on them.
As I was walking back to my vehicle to sit down in case I passed out two paramedics/firemen were running toward me. Probably the blood over my face, hair and white shirt were alarming them. They asked me to sit on their stretcher and they started to assess me: When they asked me my name, I responded, but I slurred my speech so badly they asked me if I had been drinking. It was six-thirty in the morning! And, I don't drink! He then asked me to hold his hands and squeeze them. I am generally pretty strong, especially in my left hand because I'm left handed, but I could hardly squeeze his hands. He then put his hand by the left side of my head, and asked me how many fingers he was holding up. I could not only tell how many fingers he was holding up. I couldn't clearly see his hand! I was rapidly losing my peripheral vision! He then expressed that the left side of my face was sagging.
He knew I was in serious trouble, so he asked me which hospital I wanted to go to. I told him Sunrise Hospital because I had heard from a colleague they had a good head trauma unit.
They took me in their fire truck/ ambulance to Sunrise Hospital (Which I don't remember.). The paramedic called ahead to let the personnel at Sunrise Hospital know that I was coming, so they could be ready. When I arrived a neurosurgeon, Dr. Lin, and a neurologist were waiting for me in the emergency room.
They put me on a CT scan which showed I had a blood clot in the right, rear hemisphere of my brain. Specifically, in my M2 artery. They explained to me that they couldn't give me clot busting drugs because it could cause hemorrhaging in my brain because of the severe head trauma. The only option left was a thrombectomy procedure (click here to view a YouTube video of the procedure). This procedure involved making an incision in my groin into my femoral artery, and inserting an instrument with a camera and a device to remove the clot into my femoral artery and pushing it through the artery up into my brain until they could find the blood clot and remove it. They asked me to sign some papers prior to performing this procedure. Here I am lying on my back on a stretcher, bloody, a long gash in my head, thinking I've never been in hospital, let alone know if a thrombectomy procedure is safe. I mean you're going to go into my brain with this thing! Geez! So, I said to the neurosurgeon, Dr. Lin, may I borrow your phone, so I can call my sister, Kim, who is a RN, so I can ask her if I should do this? He handed me his phone and as I was laying on a stretcher, bloody, experiencing various symptoms’ of a stroke I dialed Kim and expressed to her, "Kim, I'm in the emergency room at Sunrise Hospital in Las Vegas with a blood clot in my brain. The neurosurgeon, Dr. Lin, and the neurologist, Dr. DeAndrea want to perform a thrombectomy on me to remove the blood clot. Should I do this? Is it safe? Please call me back." I hung up the phone, and gave it back to Dr. Lin. I told him I couldn't get any feedback from someone I know and trusted, that is, my sister, Kim, so I momentarily lay there. Without skipping a beat Dr. DeAndrea, said, "If it were me I'd do it." He said that with such a calming, and trust engendering effect on me that I felt secure in signing the paper (I'm sure he was thinking something to the effect, "Seconds lost, is brain lost.). With that, I signed the paper for Dr. Lin to do the thrombectomy. They anesthetized me, and opened up my femoral artery in my groin area, so he could maneuver the device with the camera on it that would remove the blood clot. (Oh, somewhere in between entering the emergency room and now I remember someone talking to me and rummaging through my hair tracing the bleeding. They found the gash in my head and stapled it shut.) What seemed to me to be in a short time I remember Dr. Lin exclaiming, "I got it!" There was celebrating (As best I can remember being prone, and anesthetized.).
I then was moved to intensive care in the Neurosciences section of the hospital for observation, testing to attempt to determine where the blood clot came from in the first place with the intent to avoid a second stroke.
An IV was inserted into my left arm (another first for me...) which stayed there for nine days.
I basically rested for the rest of the day which was interrupted by blood tests, IV bag changes, blood pressure readings, blood draws and so forth. I was pretty much in a state of shock that all the above had happened to me, and wondering on some level if things were going to be 0.K.. I recall thinking that I had not smoked or done drugs or drank to avoid things like the above. So, I kept wondering what I had missed or what didn't I know that I should have done? Nothing was coming to me...so I just tried to relax.
I called my sisters, brother, cousins, aunts and uncle and mom.
Kim, who I had attempted to reach prior to the thrombectomy, called me back to let me know that she had got my message, and the message sounded like I was "drunk". I still was unaware of how I sounded, but I know Kim wouldn't misrepresent the way I sounded (She saved the answering machine message for evidence.). Eventually, I laughed about it, but it still is disconcerting to me that one can basically "feel" fine while simultaneously having part of your brain be in the process of dying. Maybe I still will have this disconnect forever because my only (or anyone's for that matter...) reference point - my brain - wasn't functioning well, so I couldn't cognitively appreciate that my face was drooping (left side), my speech was slurred, my peripheral vision on the left side of my head had deteriorated rapidly, and I virtually had no grip strength in my left hand and so forth.
Kim told me that Chris and she were going to fly out tomorrow, the 8th. I told her that I appreciated that, but on some level I didn't want to disrupt their work schedules, and that I felt fine. She exclaimed, "Brian, you just had a stroke!" With that, my stroke effected brain was looking forward to them being with me on Wednesday.
Kim and Chris, arrived at about 11:00 a.m. on the 8th. Dr. Zafar, my cardiologist, had done some testing on my heart on Tuesday, but didn't find evidence of any blood clots. He wanted to do another test on my heart called a Trans esophageal echocardiogram (click on Trans esophageal echocardiogram to see a YouTube video of this procedure) to look at the back side of my heart for any evidence of blood clots. Eventually, it was scheduled for Thursday, the 9th of June.
On Wednesday, June 8th, prior to Kim and Chris arriving at around five-thirty in the morning I was transported to have a MRI. That showed the area of my brain that was effected by the stroke which was minimal compared to the size of my brain tissue that would have been destroyed had Dr. Lin not removed the blood clot from my M2 artery. Because of the paramedic/fireman's training in recognizing symptoms of a stroke and his speed in getting me to the hospital, Dr. Lin’s and Dr. DeAndrea’s expertise in advising me and their skill in brain, blood clot removal I avoided being paralyzed on the left side of my body or dead. Dr. DeAndrea drew a picture of the area that would have been lost of the right hemisphere of my brain, if the blot clot had not been removed (Reference the cross-hatched area in the picture taken by Kim, below) and ,also, he drew a dark spot on my brain that the stroke had effected (Reference the dark spot adjacent to the cross-hatched area in the picture taken by Kim, below.). That dark spot represents, minimally, sixty million brain cells. A person loses approximately one million brain cells per minute while having a blood clot in their brain, which is a stroke.
Kim and Chris had to leave to go back to the airport prior to my completing the Trans esophageal echocardiogram, but as I was recovering from the procedure in the "Cath Lab” Dr. Zafar briefed Kim and Chris on what he had found. The good news: He didn’t find any evidence of any blood clots in the back side of my heart! The mixed blessing news: He found that I had a hole in my heart between my atriums (the upper chambers of my heart, and yours, too.). I'm not sure if Dr. Zafar had explained this to Chris and Kim prior to them having to leave for Des Moines, but I learned from him and others after being transported back to Neurosciences Intensive Care from the "Cath Lab” that a hole between the atriums can slow the blood flowing from the left atrium(deoxygenated blood)into the left ventricle sufficiently that a blood can form a clot which may migrate to the right atrium, and, consequently, be pumped into a person's brain(in this case that person may have been me, but because there isn't presently available instantaneous testing that can conclusively show this no one will ever know for sure, but it is reasonable to deduce that in my case that this probably was the case.). For all of you NFL fans and particularly New England Patriot fans approx. a decade ago Tedy Brushi, a linebacker for the Patriots and a University of Arizona graduate, had a stroke a couple of weeks after his third Super Bowl appearance, and after diagnosis and testing at Mass. General, the doctors there discovered that he, too, had a hole in his heart, but in Mr. Bruschi's case, his was between his ventricles or the lower chambers of his heart. Mr. Bruschi does an excellent job of detailing his experiences- his fight- through this process in his book: Never Give Up: My Stroke, My Recovery, and My Return to the NFL.
This news from Dr. Zafar was at the very, very least disconcerting. I had never heard of a PFO procedure , (click on PFO procedure to see a YouTube video of the procedure) just like I had never heard of a thrombectomy.
I wasn't really sure where to begin in deciding to have the PFO procedure or not. I knew everything in my being wasn't ready yet.
But somewhere along the line someone scheduled me for the PFO procedure on Friday, the 10th of June, 2016 @ 4:30 p.m... I was trying to get myself psyched up to do this, but I was to conflicted/unsure to proceed so, I called Ticey, my nurse practitioner. She came to my room and we talked about the pros and cons of this procedure. Using a blood thinner to cope with possible future blood clots, etc.. Even though Ticey did an excellent job of trying to help me sort through my concerns I just couldn't come to a decision that I was comfortable with, so I told Ticey I needed more time. She asked me, "How long would you like?" I said, "A couple of days to do research."
I started by calling Aunt Gretta who was a surgical nurse. She in no uncertain terms stressed that the cardiologist who would perform the procedure had to have performed it many times.
That was the first priority in selecting a cardiologist: A lot of experience with this specific procedure.
I then called my first roommate at Iowa State University who is a pathologist and a Professor of Medicine at The University of Chicago. Tony asked other doctors at the University of Chicago who had experience/ knowledge in PFO procedures. Tony called me back and told me that his colleagues had done many of these procedures, and usually, the only time doctors discover that someone even had this done is when they do an autopsy. He assured me it was safe, and that the procedure had been around awhile. Those affirmations, along with my sister, Kim, and my brother-in-law, Dennis, gave me confidence I should proceed with the procedure even though I had some reservations that were referenced in the neurology literature versus the cardiology literature. I called Stanford University, The Cleveland Clinic, Loma Linda University and others to try to more thoroughly understand the risks, if any, with the procedure, the long term consequences, while following-up on Aunt Gretta’s advice to find a cardiologist with a lot of experience in this specific procedure. The drawback with going out of state was the continual follow-up appointments in cardiology, neurology, my general practitioner, etc....
After a lengthy search from my hospital bed, a good friend of mine, Marv, called me to let me know that a close friend of his who was a Yale Medical School graduate, and a thoracic surgeon recommended Dr. Zafar. Because of my confidence that Marv was trustworthy I felt confident that staying in Las Vegas, and letting Dr. Zafar do the procedure was a wise option. That also took the burden off of me of the time and travel expenses with follow-up appointments at other out of state medical institutions.
So, with that, I had my immediate nurse call Ticey (my nurse practitioner) that I was ready to do the PFO procedure and have Dr. Zafar do it. Given I had no prior knowledge of a PFO procedure to help me make this decision I think I could have researched for the next two months and still not felt psychologically or emotionally comfortable with it. I do know one thing about it for sure: Chris, my sister, told me after the procedure that she had watched it on YouTube, and said something to the effect that, "I don't know if I'd do that!" Thank you, Chris, for your restraint by NOT telling me that until after I had gone thru the PFO procedure. I expressed that, like I said to Ticey on the 12th of June, 2016, but I don't recall anyone ever coming to my room to verify when it was going to happen on Monday, the 13th of June. I do remember that I couldn’t eat anything the night before, and until the procedure was done. I do remember that at roughly 4: 00 p.m. on the 13th two guys from the "Cath Lab"(Actually, the same two guys that had prepped me for the trans-esophageal echocardiogram.) came to my room to put me on a gurney and take me down to the "Cath Lab" to prepare me for the procedure. I still hadn't gotten a crystal clear idea of what was going to be done to me, so I asked them, and with the help of a video of the procedure while lying on the operating table I turned my head sideways to watch it while they did an excellent job of explaining. Shortly, after that, Dr. Zafar came in, cut into two of my veins in my groin and, first, inserted a camera into one vein to travel up to my heart, to determine the size of the hole between my atriums. The second incision in my groin was used to insert the correctly sized titanium device and guide it to my heart, insert it on either side of the hole between my left and right atriums, and, finally, to tighten it. When all that was done Dr. Zafar showed me the device in my heart on a jumbo size screen to my left. From my perspective it looked like two parallel wheels with a small space in between them. (Oh, I forgot to mention, one critical detail, that is, prior to inserting the camera or the properly sized titanium device between my atriums there had to be two roughly eight inch long and one-quarter inch in diameter plastic tubes (see picture, below.)
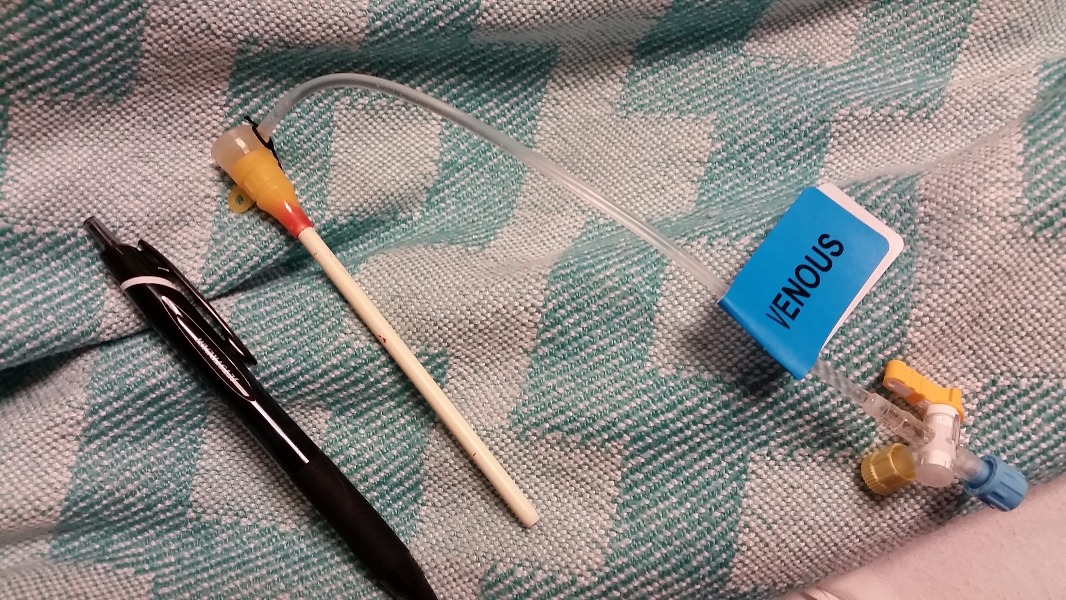
inserted in each vein to help them maintain structural rigidity enough to allow a camera or a titanium heart repair device to enter either vein.). After this I was moved from the very cold "Cath Lab” to the recovery room. Bruce, my recovery room nurse, gave me specific, very stern directions about what he and the other nurses were going to do, and what I needed to do, which was: A.) Bruce and the other nurses job: 1.) First pull out one of the plastic tubes from the vein in my groin very quickly while immediately placing heavy pressure on the incision area for twenty minutes, 2.) Then quickly pull out the other plastic tube from the other vein in my groin, and, again, place heavy pressure on it for twenty minutes, and, 3.) My part: DON'T MOVE! NOT EVEN A SMIDGEN for the next six hours! That included not lifting up my head even an inch (Or even less than an inch!)! Bruce made this unequivocally clear: If I'd move, and either or both of the incisions started to bleed the whole process would have to start again, that is, heavy pressure on each incision separately for twenty minutes each and starting the counting of the six hours from zero.
The thought of the strict tolerances for laying still, and the negative consequences, that is, twenty more minutes of pressure on each incision, and six hours of laying still was fear provoking enough not to think about it. But, trying not to think about it was a tough discipline for six hours. But, the thought of having to start all over again was worse, and sufficient motivation for me to apply extreme mental focus to lie still.
The next few days in the hospital were mostly spent walking with physical therapists, talking to a speech therapist, an occupational therapist, my internal medicine doctor, Dr. Syed, about blood thinners, etc., and I was released from the hospital on the 15th of June, 2016.
While in the hospital I told various people that my right shoulder hurt, but obviously heart and brain function took priority, so when I was trying to shower and get dressed (which I hadn’t done for nine days) I couldn’t use my right arm without severe pain. I attempted to work through that for days, but it continued to persist which brought me to the point of getting it x-rayed, and seeing my general practitioner, Dr. Miller, who referred me to an orthopedic surgeon.
I can’t have another MRI for six months because of the titanium device in my heart (The strong magnetism generated by an MRI machine can potentially dislodge the titanium device), so the orthopedic surgeon couldn’t order one of those. But, physical therapy, twice a week for the near future was prescribed. Determining positively whether or not I have a tear in a ligament, tendon and/or a muscle will have to be delayed until a more definitive diagnosis using an MRI can be done.
I will be undergoing more diagnostic measures, hopefully, in the near future to determine if I have a blood clot on the inside of my femoral artery, and/or my veins at the incision site(s) for the thrombectomy procedure and the PFO procedure. I’ve been experiencing sharp pain in this area, so it warranted being followed-up with.
Sixty-million dead brain cells had a significant function for me, but what? Even though an hour is considered a relatively quick response time for the removal of a brain, blood clot it still can cause abnormal brain function because of the sheer volumn of brain cells lost, so I am going to see a neuropsychologist for evaluation, and hopefully, establish a baseline of what psychological, emotional and physical deficits it caused, and what can be done to get those functions back to normal.
Today, 23 August, 2016 I received a new referral from my orthopedic surgeon to continue physical therapy because my shoulder is at about six percent of its normal strength. For example, I can curl only three pounds where prior to the accident I could curl fifty pounds or more.
An ophthalmologist will evaluate my peripheral vision to determine if it is sound, hopefully, in the near future. It continues to improve.
I am learning to be aware, and sensitive to what before I may have considered a small pain, and disregarded it. That learning process and follow-up will be ongoing for at least six months while I am on disability.
My immediate and long term goal is to take sound, baby steps forward. Be patient. Heal thoroughly, and build mental and physical strength gradually and prudently.
I do not have any definite timeline to be back to work, let alone any vigorous physical activity, but I am confident that Dr. Zafar, my cardiologist, Dr. DeAndre, my neurologist, Dr. Miller, my general practitioner, Tim Soder, my physical therapist and all my relatives pictured at the beginning of this (and the many more not pictured), and all my friends: Evonne and Larry, Lothar, Steven, Michael, Kathy, Karen and Erek, Stephan and Pat, Jerry, Rudy and Sabrina, and Katie C. will get me there safe and sound.
And, a uniquely, special thanks to Tedy Bruschi and his wife, Heidi, for your heartfelt care and concern and unselfish forsight to want to share the details of your stroke experience with the hope that it would provide encouragement, and hope for a full recovery to all those experiencing one. I asked Dr. Zafar at some point in this process, if he ever thought that I could run, again. The first thing out of his mouth was your name, that you had experienced a stroke and a PFO procedure, and had rehabilitated and returned to the NFL. The NFL has never been part of my job description, so returning to it won't be one of my goals, but running a roadrace like Falmouth, hopefully, someday will be.
Thankyou, infinitely, for and to the Creator of all life, Jesus of Nazareth for without Him even the possibility of generating thoughts, let alone thoughts about one of HIS creations, our brains, wouldn't exist.
Sincerely,
Brian


