
Kenya Australia Nurse Education
Donation protected
Kenya Australia Twinning Project
Stoma, Wound and Continence Nursing
Education Program (SWCNEP)

Australian Stomal Therapy Nurses train their Kenyan Colleagues
The program has already improved the health and welfare of people with stomas wounds and incontinence
Help to keep the Program running
********************************************************
Information
A stoma or ostomy is a surgically created opening on the abdomen for the elimination of faeces or urine. A person with a stoma in a developed country such as Australia wears a disposable ostomy bag for the collection of waste and is able to enjoy a good quality of life. Unfortunately people in developing countries who have a stoma because of disease, congenital abnormality or trauma usually have to cope with the stigma, the odour, the containment in a less than desirable manner and with minimal assistance.
This is the story of a Twinning Project between Australia and Kenya to develop specialist nurse training in Africa to care for individuals with stoma, wound or continence needs.
The initial request for stoma education in Kenya came to the World Council of Enterostomal Therapists (WCET) from the Aga Khan University Hospital Nairobi. Nurses in Kenya identified they had limited knowledge to adequately care for individuals with intimate health care needs especially those with stomas.
Stomal Therapy Nurse Elizabeth English, from the Royal Adelaide Hospital, South Australia and an active member of the Australian Association of Stomal Therapy Nursing (AASTN) was the WCET President at the time.
It was arranged for Prilli Stevens a well renowned stoma nurse from Cape Town South Africa and life member and past President of WCET to be supported by WCET to travel to Nairobi and conduct a short course in stoma care.
From there the seed was sewn.
Elizabeth taught another short education program in 2011 and it became evident to her that Kenya was ripe for the development of a formal WCET-recognised Stoma Wound and Continence Nursing Education Program (SWCNEP).
With the help of Carmen George, WCET Education Committee Chairperson at the time submissions were written and funding sought and a proposed program was submitted to the WCET for recognition.
ConvaTec had generously given WCET Norma N Gill Foundation US$20,000 in the hope that this could be used to support Kenya and, in an act of faith, Elizabeth wrote to the Australian Association of Stomal Therapy Nurses (AASTN) Executive for their support. An email was sent to all members requesting Stomal Therapy Nurse (STN)volunteers to assist in conducting a program. The response was overwhelming; however, with only US$20,000 as backup, only those STNs who could commit to four weeks for the first module
in October–November 2013 were chosen. Fundraising was then started in earnest, with the AASTN Executive and some state branches being generous donors. Other donors also generously contributed in paving the way for the dream to become a reality
The following is a report about the journey
In October 2013 the first module of the first SWCNEP in Kenya began with 20 students – 18 from Kenya and 2 from Tanzania.….hosted by the AKUH.
An initial problem was obtaining a classroom big enough to house the 20 students as well as the tutors. Often we met in a small classroom in the morning and then walked down the busy road to a rooftop space owned by the university for the afternoon sessions. Some activities such as stoma site selection and teaching regarding turning and positioning a patient were conducted outside on the lawn!! (the gardens, trees and flowers are beautiful in Kenya : a sharp contract to the dusty crowded hazardous roads.)
Two months prior to our arrival, members of extremist Islamist group al-Shabaab, armed with assault rifles and grenades had attacked the local Westgate shopping mall, killing 67 people and seriously wounding 175. We were well aware that Nairobi is not a safe place but we were not daunted, we had work to do.
The main place for our clinical visits was the Kenyatta National Hospital, a 2000-bed public hospital in Nairobi — the biggest referral hospital in East and Central Africa — often with an occupancy rate of 3000, with two patients to a bed or mattresses
on the floor. It has 600,000 outpatient visits a year and 90,000 inpatients a year, with daily public traffic of 30,000. Initially, it was thought that we could just pop down the road to Kenyatta for clinical experience, but it was not so simple. Due to security,we needed to go in a chartered bus and, because of the traffic jams, the ride was at least an hour, sometimes more.
Visiting this huge hospital was an experience. Sometimes the magnitude of the patient’s problem was overwhelming and we had to take a deep breath before contemplating the next move. There were minimal hand-washing facilities; no pillows; thin, vinyl-covered mattresses; a minimal supply of sheets;
no supplies except those we had brought with us — yet there was dedication by the doctors and nurses, who were doing the best they could with the lack of resources and manpower. The patients, despite minimal comforts and often-inadequate pain relief, were uncomplaining. We could have worked 24 hours a day, seven days a week and still there would be more to do.
It was incredible to see the number of ARMs (anorectal malformations) — wards full of mothers with babies born without an anus with colostomies. Wards full of people who had been burnt — many of them children — their kerosene fires used for cooking either blow up, or the children fall into the fire. We
saw men who had been working on the roads burnt with hot tar,some from industrial accidents, others from cooking fires. We saw so many congenital abnormalities such as cloaca, tracheo-oesophageal
fistula, gastroschisis, omphalocele, Hirschsprung’s
disease. We looked after those with HIV complications, typhoid perforations, sarcomas, fungating cancers of all types, and accident victims with paraplegia with the worst pressure injuries.
Osteomyelitis seemed a common condition. The outpatient and casualty departments were always crowded. A sea of black faces just sitting there, patiently waiting, waiting. The outside lawns
and walls were also usually crowded with more people, also waiting.
We also went to Kijabe Mission Hospital, in the Rift Valley outside of Nairobi. . We found the clinical experience at Kijabe confronting and challenging. We encountered diseases only known to many of us through textbooks: for example, typhoid,TB, malaria, HIV, schistosomiasis, filariasis. We were confronted by irreparable pressure injuries and traumatic wounds. Kijabe has the biggest population of children with hydrocephalus.There were stoma patients coping without stoma bags, people presenting with metastasising cancers, diabetic ulcers, infected
wounds, anything and everything — yet all patients were stoic and uncomplaining..
It was uncanny at times how things just happened. Although repeat outpatient visits sometimes could not be planned, if the patients knew when we would be returning, they sometimes just turned up and would somehow find us (although I suppose as a mzungu [white person] we did stand out in the crowd!).
At times we faced an ethical dilemma — what to use on huge wounds.
Should we use large amounts of donated Western dressings,knowing that this practice would be unsustainable once supplies were exhausted?
Should we use best practice and see what we
could achieve in the short time we had access to that patient?
There were many success stories. However, there were other situations where using the local, cheap, sustainable products, for example, honey bought from the supermarket, had equally positive outcomes. Nurses in the ward were always interested in what we were doing and, with beds packed close together,
crowd control became an issue.
 2014 students all received a donated USB
2014 students all received a donated USB
The 2013/2014 program set the scene with its 20 graduates and plans then centred on preparing for the next program.
The 2015 program had 19 Kenyan nurses from places all around Kenya plus one nurse from Togo.
Vincent the bilingual nurse from Togo gained a WCET scholarship to attend the program. He is already being mentored by the French speaking Swiss WCET stoma nurses so he will be a wonderful resource to the French speaking people of western Africa and has already travelled to Cameroon and Mali.
Three other students from Nairobi also gained WCET scholarships, four were supported by international grants available to AKUH and our general fund paid a proportion of costs for three nurses from the Kijabe Mission Hospital and contributed to accommodation costs for the remote Kenyan tutors for the final module.
A new project such as this always has a learning curve and the 2015 program certainly was challenging. Trying to work on a smaller budget for the second and third modules with less tutors was not ideal with tutors finding the individual work load hard going. Trying to plan and negotiate from afar is never easy but one must always be respectful and cognisant of the cultural aspects and the politics involved – however despite the difficulties, the outcome was very positive
A great achievement was seeing seven of the 2014 graduates returning to volunteer and be mentored as tutors in future programs. They acquired the name of the KTs – the Kenyan Tutors and were invaluable in the assistance they gave the Australian tutors during the 2015 program.
Five of the KTs gained WCET Congress Scholarships to enable them to travel to Cape Town, South Africa to attend the WCET Congress in March 2016. They were the very excited, newly appointed Kenyan International Delegate (ID) Christine Mutuku from Kijabe, Jane Ndungu from Kenyatta National Hospital, Alice Zachary from Kisii, Lydia Omari from Wajir and Imelda Makokha from Kisumu.
 Australian WCET International Delegate Sharon Boxall and Kenyan International Delegate Christine Mutuku in national costume for the Parade of Nations at the WCET Congress in South Africa 2016
Australian WCET International Delegate Sharon Boxall and Kenyan International Delegate Christine Mutuku in national costume for the Parade of Nations at the WCET Congress in South Africa 2016
Harriet Ibaya would have loved to attend (and had her abstract accepted as did Grace Wanyoike a student from 2015 and a NNGF scholarship recipient, but neither could get hospital support for leave).
Jane Ndungu confidently presented a paper on the developments in stoma, wound and continence care at the Kenyatta National Hospital and I introduced the five KTs in my presentation titled Kenya is Awakening.
 Jane Ndungu with Elizabeth English and WCET Life members Prilli Stevens and Marylyn McManus at the WCET congress 2016
Jane Ndungu with Elizabeth English and WCET Life members Prilli Stevens and Marylyn McManus at the WCET congress 2016

4 of the KTs Imelda, Alice, Lydia and Jane
Kenyatta National Hospital once again opened its doors to us with a room being provided for handover and enough patients to keep us with clinical work 24/7. One 35 bed orthopaedic ward had 115 patients! We even saw three to a bed with two per bed common throughout the ward. As before it was an incredible experience having the privilege to assist nurses develop specialised care for a wide range of patients in need.
Kenyatta had five students in the 2015 program and with Jane from the first program this busy hospital now has a strong team of six SWC nurses - all of them so keen to make a difference in the biggest hospital in Kenya. Jane together with new graduate Grace already conduct ward rounds, regular outpatient clinics, a monthly ostomy support group and accept referrals. This is an amazing achievement in just one year!
Kijabe Mission Hospital hopefully will again be a clinical partner in 2016, as it was in 2014 with costs for transport of students and tutors factored into the budget. We did visit once in 2015 but a change in the weather forced us to make a hasty retreat. Despite this the bus still managed to get bogged precariously off the side of the rain affected dirt, country road leaving more than 20 of us stranded in the rain with daylight diminishing and the fog setting in. After hours of unsuccessful activities trying to get the bus back on the road, further negotiation saw us all being loaded in our dampened state into the back of an open tray cattle truck and with standing room only and hanging on to the roll bars, we began the precarious chilly trip in the fog, up the muddy road, with the hillside dipping away at the side, and multiple other vehicles bogged and semi blocking our path. A little hair-raising to say the least but there was more fun to be had. Arriving at the main highway we then had to disembark the truck (not easy when one is old and grey!!) and take our life in our hands to cross the main highway to the matatu (think mini van) bus stop. It was dark by this time but fortunately the students took charge and ensured we were packed into the correct matatu. Then began another hair-raising event in the battered combi-van type mini bus with no seatbelts, a kamikaze driver with minimal English, who drove us home at breakneck speed on a multi laned, dimly lit, crowded highway. We have been “God blessed” so many times in Kenya and that was one time that we really hoped the blessings would hold. We survived and didn’t even get pneumonia!!
2016
Plans for the 2016 program are underway. This is the final year in the three year Twinning project with the first module beginning in August 2016 for three weeks and the second and third modules in January/February and May 2017. Tutors who have previously been involved are once again volunteering with several extra STNs invited to fulfil special aspects of the program.
The Aga Khan University Hospital School of Nursing has agreed to make the 2016 program a continuing professional development program and thus a definite classroom has been secured ahead of time for the 2016 class. The hospital has also recognised the worth of our training and a wound care nurse position has been set up for a graduate of the 2014 SWCNEP to conduct a regular wound clinic which is well patronised by medical and nursing staff of the AKUH.
The main aim of this project was to have a sustainable program conducted by Kenyan nurses in the fourth year and thereafter. This now appears to be achievable with medical and nursing administrative personnel being supportive. A week of master classes has been planned for January 2017 for graduates of 2014 and 2015. This will be an AASTN initiative conducted separately but at the same time as the basic program’s second module. Keryln Carville and Vicki Patton will be responsible for this program while other tutors will concentrate on students in the basic program. There is already interest from Botswana, Namibia, Rwanda, Uganda and Tanzania so the word is spreading about our speciality of nursing and the Kenyan SWCNEP
Once again there were memorable events for all tutors in the program. One of my favourite patients who now writes to me, has asked in his last letter if I could get him a table on which to do his homework otherwise he has to do it on the bed which he shares with other members of his family. Only problem is, in his tiny little dwelling there is no place to put the table so he wonders if he could get a new house for him, his widowed mother and 3 siblings! I had told him to think positive and that a stoma will not stop him from fulfilling his dreams and reaching his goals so he is obviously acting on that advice! Unfortunately his recent pull through operation (which he should have had done early in life) was not successful as he was lost to follow up when young because his family could not afford hospital treatment or the fare to Nairobi. Consequently his Hirschsprungs affected colon has deteriorated markedly over the years making surgical reconstruction unsuccessful. He now has a stoma for life, but donated bags will at least give him a far better quality of life than the binder he wore previously. (He is the boy who gazed with wonder at the shopping mall when we took him for a shopping excursion and gurgled with delight when he went for his first ride (at the age of 15! ) on an escalator (the moving staircase) and instead of wanting the type of present our Australian young people would like, he humbly asked for black lace up school shoes!!
My other little delight is a 12 year old girl born with an anorectal malformation with vaginal fistula who had a stoma at birth and was ostracised because of the smell and “being different” so became illiterate as she was not allowed to go to school. A “good Samaritan” brought her into the Kenyatta Hospital. She was small for her age because of lack of food, her only dress was soiled with faeces and she was frightened. The students were so kind and spoke to her in Swahili to explain our role and tell her not to be frightened of the Mzungu (the white foreigner). They showed her ostomy bags and how to cut out the hole. She managed OK but was still obviously apprehensive. Then the bag was applied, slowly she appeared to realise that perhaps this would prevent odour and leakage. Suddenly a huge smile spread across her face. The paediatrician was amazing, plans were made to admit her immediately for surgical reconstruction, the social worker was involved to admit her as a charity case and the woman who had brought her to the hospital stated she would continue to look after her following discharge from hospital. She was enrolled in the beginner class at the hospital school and every day after that when I walked into the paediatric ward a little figure would come running toward me with a big smile and a huge hug. She was able to write her name by the time I left and was loving school. She underwent surgical repair, still has her stoma but in time the stoma will be closed and she should be able to function normally. Her carer (who turned out to be the wife of a pastor) has emailed me to say “The child is doing well. We love her. She is going to read to you in English when you come back in August. There is now no more stigma. She is getting the education she yearned for.” How blessed am I to have met this dear little girl.
There are so many other stories – many not as happy as the last but to know that our endeavours are definitely making a difference makes it all worthwhile.
This program would not have been possible without the support of generous donors plus the wonderful, hardworking AASTN team members Vicki Patton, Trish Griffin and Sharon Boxall who have been involved with me in both programs and Helen Richards, Keryln Carville, Jenny O’Donnell, Ann Bew, Emma Vernon, Sheryl Waye, Leigh Davis, Helma Riddell, Nobuko Murphy, Sandy Hyde-Smith and Sharmaine Peterson. A big thank you to all for your commitment. We are passionate, we are persistent and we do have the vision and strongly believe that this commitment has not been in vain. We have faith in our Kenyan colleagues to follow in our footsteps.
Thank you to everyone for supporting the vision for Kenya. Please have faith and continue to support us as we mentor our Kenyan colleagues so that they can give their patients the expert care that African people with stoma wound and continence needs rightfully deserve.
Sincerely - Elizabeth English Team Leader SWCNEP
Our motto Passion.... Persistence....Vision
The following are evaluation comments from students of the 2015 Kenyan SWCNEP
-Started empty on knowledge. Look at me now knowledgeable, confident and competent
-The Australian tutors were a blessing to us. Your effort will not be in vain.
-Clinical provided such exposure for me and it was awesome.
-Life changing course.
-It made an impact on me and I will transfer the impact to my country
-I am a better nurse now
-Tutors all brilliant and friendly. Very helpful. Has changed my whole perspective
-Grateful that whole team from Australia has been able to push through many obstacles to make sure the program went well
God bless you all
-I promise to continue practising the knowledge I have received.
-I didn’t know much about computers – now I can type my own assignments
-Improved my confidence in talking in front of people. – thanks to the oral presentations in class
-I am equipped with new knowledge now I need experience
-I have new friends from all over Kenya and Australia
-I have achieved more than I thought – came completely blank now have the knowledge that I would not have been able to get anywhere else.
-I have learnt such a lot
-Course really meaningful and very constructive
-I now know how to write an abstract, do a case study pictorial, power-point and present with ease.
-Now a full member of WCET and marketable to the world
-Have learnt innovation skills – to manage leaking wounds and fistula and can now deliver quality nursing care
-I can now deliver care not just in the ward but to the whole hospital
-The program is well organised and educative
-Did not think much about incontinence – now I need to take a different focus.
-I have achieved my objectives and can now mentor others with the knowledge I have gained.
-I am forever grateful for being given this chance. -God bless all the Australians
 2014 students practising with a doppler
2014 students practising with a doppler
 2014 Team members presenting text book and doll with a stoma to Kijabe Hospital SWC Nurses Grace and Christine
2014 Team members presenting text book and doll with a stoma to Kijabe Hospital SWC Nurses Grace and Christine
 2014 Graduation
2014 Graduation
 2015 students hard at work in classroom
2015 students hard at work in classroom
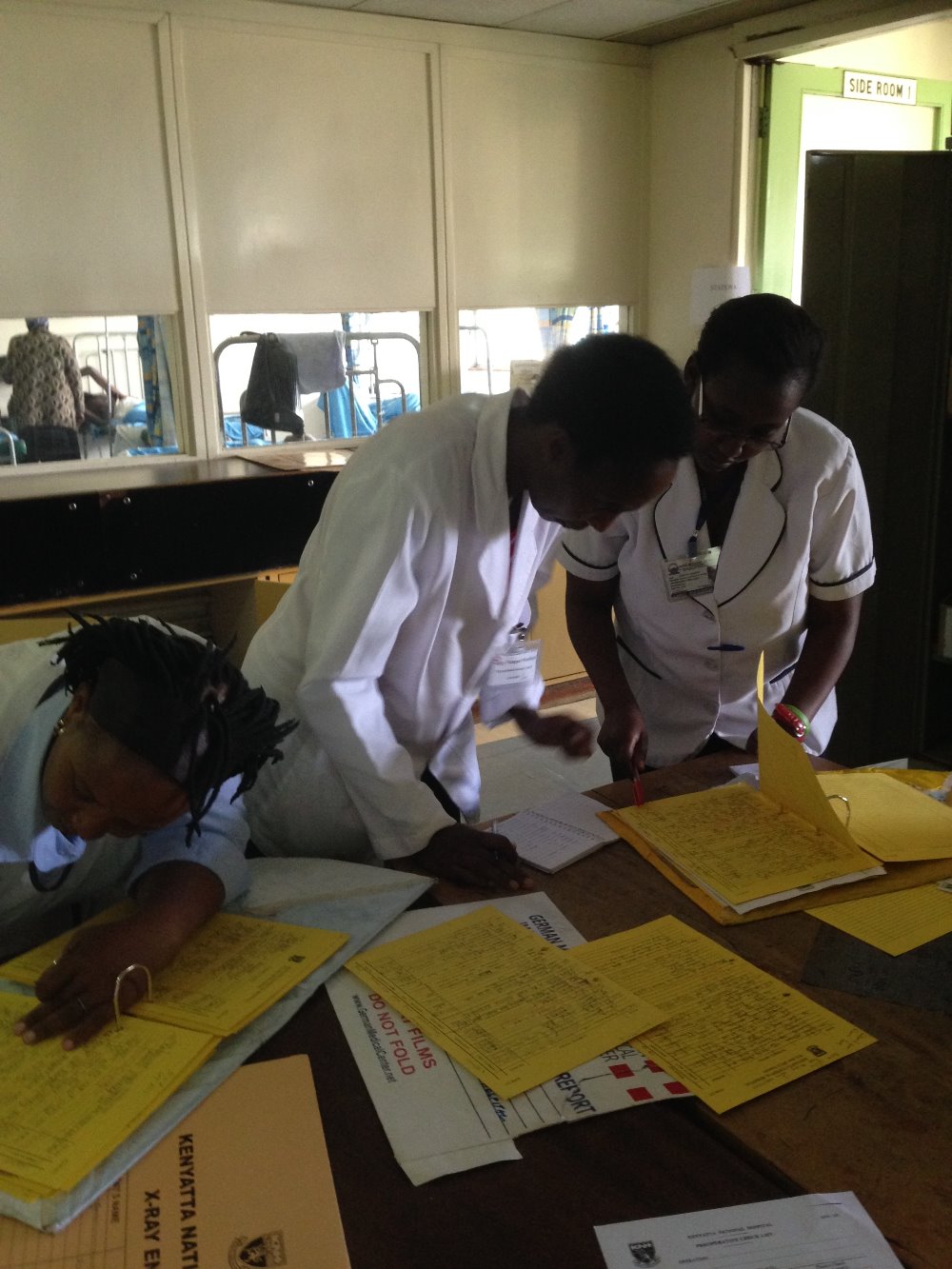
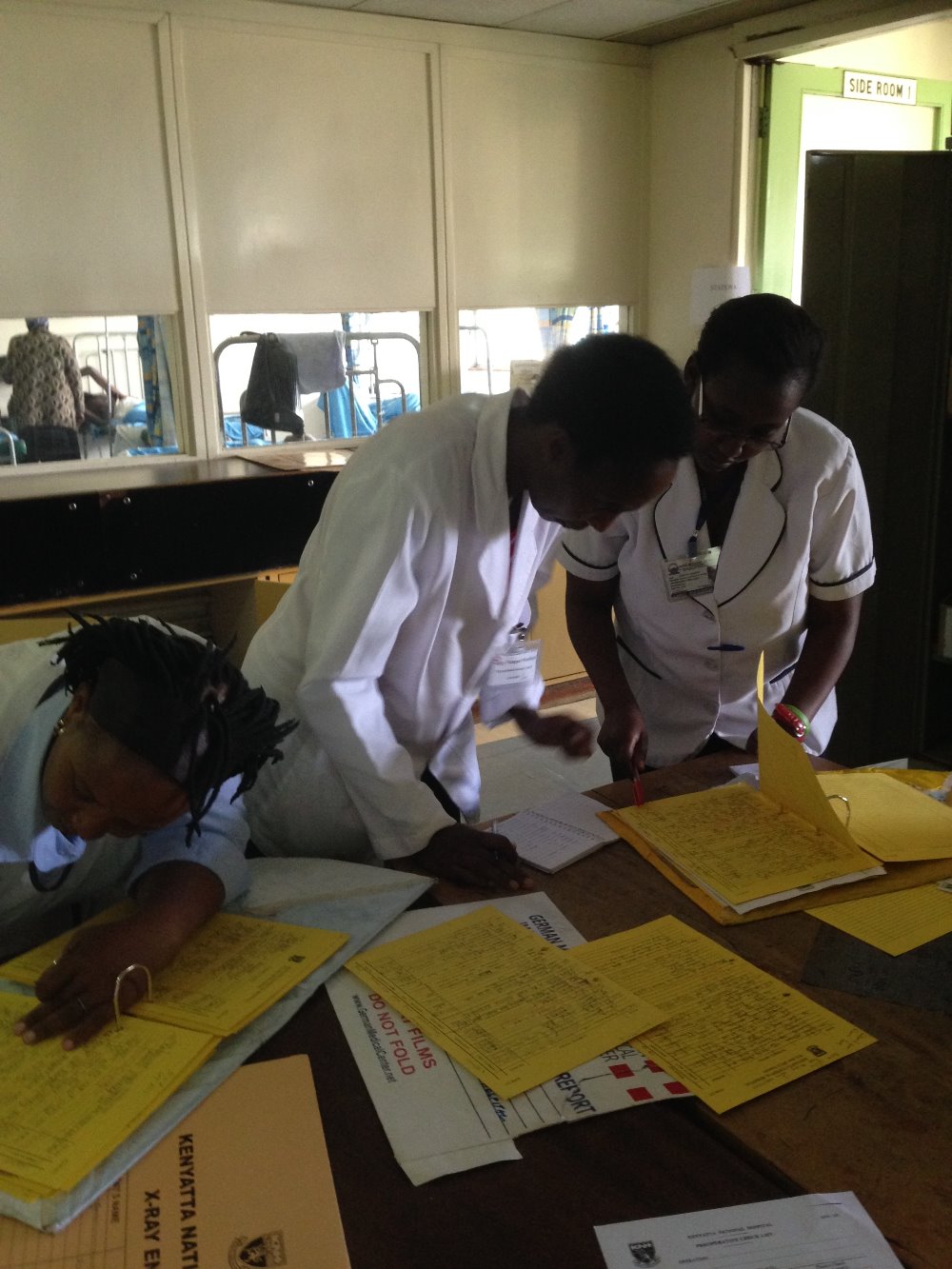
 2015 students discussing a patient at the bedside
2015 students discussing a patient at the bedside
 Wound care
Wound care
.
 Crowded ward
Crowded ward

 Being loaded on to cattle truck after bus bogged on Kijabe road
Being loaded on to cattle truck after bus bogged on Kijabe road
 2015 students
2015 students
Stoma, Wound and Continence Nursing
Education Program (SWCNEP)

Australian Stomal Therapy Nurses train their Kenyan Colleagues
The program has already improved the health and welfare of people with stomas wounds and incontinence
Help to keep the Program running
********************************************************
Information
A stoma or ostomy is a surgically created opening on the abdomen for the elimination of faeces or urine. A person with a stoma in a developed country such as Australia wears a disposable ostomy bag for the collection of waste and is able to enjoy a good quality of life. Unfortunately people in developing countries who have a stoma because of disease, congenital abnormality or trauma usually have to cope with the stigma, the odour, the containment in a less than desirable manner and with minimal assistance.
This is the story of a Twinning Project between Australia and Kenya to develop specialist nurse training in Africa to care for individuals with stoma, wound or continence needs.
The initial request for stoma education in Kenya came to the World Council of Enterostomal Therapists (WCET) from the Aga Khan University Hospital Nairobi. Nurses in Kenya identified they had limited knowledge to adequately care for individuals with intimate health care needs especially those with stomas.
Stomal Therapy Nurse Elizabeth English, from the Royal Adelaide Hospital, South Australia and an active member of the Australian Association of Stomal Therapy Nursing (AASTN) was the WCET President at the time.
It was arranged for Prilli Stevens a well renowned stoma nurse from Cape Town South Africa and life member and past President of WCET to be supported by WCET to travel to Nairobi and conduct a short course in stoma care.
From there the seed was sewn.
Elizabeth taught another short education program in 2011 and it became evident to her that Kenya was ripe for the development of a formal WCET-recognised Stoma Wound and Continence Nursing Education Program (SWCNEP).
With the help of Carmen George, WCET Education Committee Chairperson at the time submissions were written and funding sought and a proposed program was submitted to the WCET for recognition.
ConvaTec had generously given WCET Norma N Gill Foundation US$20,000 in the hope that this could be used to support Kenya and, in an act of faith, Elizabeth wrote to the Australian Association of Stomal Therapy Nurses (AASTN) Executive for their support. An email was sent to all members requesting Stomal Therapy Nurse (STN)volunteers to assist in conducting a program. The response was overwhelming; however, with only US$20,000 as backup, only those STNs who could commit to four weeks for the first module
in October–November 2013 were chosen. Fundraising was then started in earnest, with the AASTN Executive and some state branches being generous donors. Other donors also generously contributed in paving the way for the dream to become a reality
The following is a report about the journey
In October 2013 the first module of the first SWCNEP in Kenya began with 20 students – 18 from Kenya and 2 from Tanzania.….hosted by the AKUH.
An initial problem was obtaining a classroom big enough to house the 20 students as well as the tutors. Often we met in a small classroom in the morning and then walked down the busy road to a rooftop space owned by the university for the afternoon sessions. Some activities such as stoma site selection and teaching regarding turning and positioning a patient were conducted outside on the lawn!! (the gardens, trees and flowers are beautiful in Kenya : a sharp contract to the dusty crowded hazardous roads.)
Two months prior to our arrival, members of extremist Islamist group al-Shabaab, armed with assault rifles and grenades had attacked the local Westgate shopping mall, killing 67 people and seriously wounding 175. We were well aware that Nairobi is not a safe place but we were not daunted, we had work to do.
The main place for our clinical visits was the Kenyatta National Hospital, a 2000-bed public hospital in Nairobi — the biggest referral hospital in East and Central Africa — often with an occupancy rate of 3000, with two patients to a bed or mattresses
on the floor. It has 600,000 outpatient visits a year and 90,000 inpatients a year, with daily public traffic of 30,000. Initially, it was thought that we could just pop down the road to Kenyatta for clinical experience, but it was not so simple. Due to security,we needed to go in a chartered bus and, because of the traffic jams, the ride was at least an hour, sometimes more.
Visiting this huge hospital was an experience. Sometimes the magnitude of the patient’s problem was overwhelming and we had to take a deep breath before contemplating the next move. There were minimal hand-washing facilities; no pillows; thin, vinyl-covered mattresses; a minimal supply of sheets;
no supplies except those we had brought with us — yet there was dedication by the doctors and nurses, who were doing the best they could with the lack of resources and manpower. The patients, despite minimal comforts and often-inadequate pain relief, were uncomplaining. We could have worked 24 hours a day, seven days a week and still there would be more to do.
It was incredible to see the number of ARMs (anorectal malformations) — wards full of mothers with babies born without an anus with colostomies. Wards full of people who had been burnt — many of them children — their kerosene fires used for cooking either blow up, or the children fall into the fire. We
saw men who had been working on the roads burnt with hot tar,some from industrial accidents, others from cooking fires. We saw so many congenital abnormalities such as cloaca, tracheo-oesophageal
fistula, gastroschisis, omphalocele, Hirschsprung’s
disease. We looked after those with HIV complications, typhoid perforations, sarcomas, fungating cancers of all types, and accident victims with paraplegia with the worst pressure injuries.
Osteomyelitis seemed a common condition. The outpatient and casualty departments were always crowded. A sea of black faces just sitting there, patiently waiting, waiting. The outside lawns
and walls were also usually crowded with more people, also waiting.
We also went to Kijabe Mission Hospital, in the Rift Valley outside of Nairobi. . We found the clinical experience at Kijabe confronting and challenging. We encountered diseases only known to many of us through textbooks: for example, typhoid,TB, malaria, HIV, schistosomiasis, filariasis. We were confronted by irreparable pressure injuries and traumatic wounds. Kijabe has the biggest population of children with hydrocephalus.There were stoma patients coping without stoma bags, people presenting with metastasising cancers, diabetic ulcers, infected
wounds, anything and everything — yet all patients were stoic and uncomplaining..
It was uncanny at times how things just happened. Although repeat outpatient visits sometimes could not be planned, if the patients knew when we would be returning, they sometimes just turned up and would somehow find us (although I suppose as a mzungu [white person] we did stand out in the crowd!).
At times we faced an ethical dilemma — what to use on huge wounds.
Should we use large amounts of donated Western dressings,knowing that this practice would be unsustainable once supplies were exhausted?
Should we use best practice and see what we
could achieve in the short time we had access to that patient?
There were many success stories. However, there were other situations where using the local, cheap, sustainable products, for example, honey bought from the supermarket, had equally positive outcomes. Nurses in the ward were always interested in what we were doing and, with beds packed close together,
crowd control became an issue.
 2014 students all received a donated USB
2014 students all received a donated USBThe 2013/2014 program set the scene with its 20 graduates and plans then centred on preparing for the next program.
The 2015 program had 19 Kenyan nurses from places all around Kenya plus one nurse from Togo.
Vincent the bilingual nurse from Togo gained a WCET scholarship to attend the program. He is already being mentored by the French speaking Swiss WCET stoma nurses so he will be a wonderful resource to the French speaking people of western Africa and has already travelled to Cameroon and Mali.
Three other students from Nairobi also gained WCET scholarships, four were supported by international grants available to AKUH and our general fund paid a proportion of costs for three nurses from the Kijabe Mission Hospital and contributed to accommodation costs for the remote Kenyan tutors for the final module.
A new project such as this always has a learning curve and the 2015 program certainly was challenging. Trying to work on a smaller budget for the second and third modules with less tutors was not ideal with tutors finding the individual work load hard going. Trying to plan and negotiate from afar is never easy but one must always be respectful and cognisant of the cultural aspects and the politics involved – however despite the difficulties, the outcome was very positive
A great achievement was seeing seven of the 2014 graduates returning to volunteer and be mentored as tutors in future programs. They acquired the name of the KTs – the Kenyan Tutors and were invaluable in the assistance they gave the Australian tutors during the 2015 program.
Five of the KTs gained WCET Congress Scholarships to enable them to travel to Cape Town, South Africa to attend the WCET Congress in March 2016. They were the very excited, newly appointed Kenyan International Delegate (ID) Christine Mutuku from Kijabe, Jane Ndungu from Kenyatta National Hospital, Alice Zachary from Kisii, Lydia Omari from Wajir and Imelda Makokha from Kisumu.
 Australian WCET International Delegate Sharon Boxall and Kenyan International Delegate Christine Mutuku in national costume for the Parade of Nations at the WCET Congress in South Africa 2016
Australian WCET International Delegate Sharon Boxall and Kenyan International Delegate Christine Mutuku in national costume for the Parade of Nations at the WCET Congress in South Africa 2016Harriet Ibaya would have loved to attend (and had her abstract accepted as did Grace Wanyoike a student from 2015 and a NNGF scholarship recipient, but neither could get hospital support for leave).
Jane Ndungu confidently presented a paper on the developments in stoma, wound and continence care at the Kenyatta National Hospital and I introduced the five KTs in my presentation titled Kenya is Awakening.
 Jane Ndungu with Elizabeth English and WCET Life members Prilli Stevens and Marylyn McManus at the WCET congress 2016
Jane Ndungu with Elizabeth English and WCET Life members Prilli Stevens and Marylyn McManus at the WCET congress 2016
4 of the KTs Imelda, Alice, Lydia and Jane
Kenyatta National Hospital once again opened its doors to us with a room being provided for handover and enough patients to keep us with clinical work 24/7. One 35 bed orthopaedic ward had 115 patients! We even saw three to a bed with two per bed common throughout the ward. As before it was an incredible experience having the privilege to assist nurses develop specialised care for a wide range of patients in need.
Kenyatta had five students in the 2015 program and with Jane from the first program this busy hospital now has a strong team of six SWC nurses - all of them so keen to make a difference in the biggest hospital in Kenya. Jane together with new graduate Grace already conduct ward rounds, regular outpatient clinics, a monthly ostomy support group and accept referrals. This is an amazing achievement in just one year!
Kijabe Mission Hospital hopefully will again be a clinical partner in 2016, as it was in 2014 with costs for transport of students and tutors factored into the budget. We did visit once in 2015 but a change in the weather forced us to make a hasty retreat. Despite this the bus still managed to get bogged precariously off the side of the rain affected dirt, country road leaving more than 20 of us stranded in the rain with daylight diminishing and the fog setting in. After hours of unsuccessful activities trying to get the bus back on the road, further negotiation saw us all being loaded in our dampened state into the back of an open tray cattle truck and with standing room only and hanging on to the roll bars, we began the precarious chilly trip in the fog, up the muddy road, with the hillside dipping away at the side, and multiple other vehicles bogged and semi blocking our path. A little hair-raising to say the least but there was more fun to be had. Arriving at the main highway we then had to disembark the truck (not easy when one is old and grey!!) and take our life in our hands to cross the main highway to the matatu (think mini van) bus stop. It was dark by this time but fortunately the students took charge and ensured we were packed into the correct matatu. Then began another hair-raising event in the battered combi-van type mini bus with no seatbelts, a kamikaze driver with minimal English, who drove us home at breakneck speed on a multi laned, dimly lit, crowded highway. We have been “God blessed” so many times in Kenya and that was one time that we really hoped the blessings would hold. We survived and didn’t even get pneumonia!!
2016
Plans for the 2016 program are underway. This is the final year in the three year Twinning project with the first module beginning in August 2016 for three weeks and the second and third modules in January/February and May 2017. Tutors who have previously been involved are once again volunteering with several extra STNs invited to fulfil special aspects of the program.
The Aga Khan University Hospital School of Nursing has agreed to make the 2016 program a continuing professional development program and thus a definite classroom has been secured ahead of time for the 2016 class. The hospital has also recognised the worth of our training and a wound care nurse position has been set up for a graduate of the 2014 SWCNEP to conduct a regular wound clinic which is well patronised by medical and nursing staff of the AKUH.
The main aim of this project was to have a sustainable program conducted by Kenyan nurses in the fourth year and thereafter. This now appears to be achievable with medical and nursing administrative personnel being supportive. A week of master classes has been planned for January 2017 for graduates of 2014 and 2015. This will be an AASTN initiative conducted separately but at the same time as the basic program’s second module. Keryln Carville and Vicki Patton will be responsible for this program while other tutors will concentrate on students in the basic program. There is already interest from Botswana, Namibia, Rwanda, Uganda and Tanzania so the word is spreading about our speciality of nursing and the Kenyan SWCNEP
Once again there were memorable events for all tutors in the program. One of my favourite patients who now writes to me, has asked in his last letter if I could get him a table on which to do his homework otherwise he has to do it on the bed which he shares with other members of his family. Only problem is, in his tiny little dwelling there is no place to put the table so he wonders if he could get a new house for him, his widowed mother and 3 siblings! I had told him to think positive and that a stoma will not stop him from fulfilling his dreams and reaching his goals so he is obviously acting on that advice! Unfortunately his recent pull through operation (which he should have had done early in life) was not successful as he was lost to follow up when young because his family could not afford hospital treatment or the fare to Nairobi. Consequently his Hirschsprungs affected colon has deteriorated markedly over the years making surgical reconstruction unsuccessful. He now has a stoma for life, but donated bags will at least give him a far better quality of life than the binder he wore previously. (He is the boy who gazed with wonder at the shopping mall when we took him for a shopping excursion and gurgled with delight when he went for his first ride (at the age of 15! ) on an escalator (the moving staircase) and instead of wanting the type of present our Australian young people would like, he humbly asked for black lace up school shoes!!
My other little delight is a 12 year old girl born with an anorectal malformation with vaginal fistula who had a stoma at birth and was ostracised because of the smell and “being different” so became illiterate as she was not allowed to go to school. A “good Samaritan” brought her into the Kenyatta Hospital. She was small for her age because of lack of food, her only dress was soiled with faeces and she was frightened. The students were so kind and spoke to her in Swahili to explain our role and tell her not to be frightened of the Mzungu (the white foreigner). They showed her ostomy bags and how to cut out the hole. She managed OK but was still obviously apprehensive. Then the bag was applied, slowly she appeared to realise that perhaps this would prevent odour and leakage. Suddenly a huge smile spread across her face. The paediatrician was amazing, plans were made to admit her immediately for surgical reconstruction, the social worker was involved to admit her as a charity case and the woman who had brought her to the hospital stated she would continue to look after her following discharge from hospital. She was enrolled in the beginner class at the hospital school and every day after that when I walked into the paediatric ward a little figure would come running toward me with a big smile and a huge hug. She was able to write her name by the time I left and was loving school. She underwent surgical repair, still has her stoma but in time the stoma will be closed and she should be able to function normally. Her carer (who turned out to be the wife of a pastor) has emailed me to say “The child is doing well. We love her. She is going to read to you in English when you come back in August. There is now no more stigma. She is getting the education she yearned for.” How blessed am I to have met this dear little girl.
There are so many other stories – many not as happy as the last but to know that our endeavours are definitely making a difference makes it all worthwhile.
This program would not have been possible without the support of generous donors plus the wonderful, hardworking AASTN team members Vicki Patton, Trish Griffin and Sharon Boxall who have been involved with me in both programs and Helen Richards, Keryln Carville, Jenny O’Donnell, Ann Bew, Emma Vernon, Sheryl Waye, Leigh Davis, Helma Riddell, Nobuko Murphy, Sandy Hyde-Smith and Sharmaine Peterson. A big thank you to all for your commitment. We are passionate, we are persistent and we do have the vision and strongly believe that this commitment has not been in vain. We have faith in our Kenyan colleagues to follow in our footsteps.
Thank you to everyone for supporting the vision for Kenya. Please have faith and continue to support us as we mentor our Kenyan colleagues so that they can give their patients the expert care that African people with stoma wound and continence needs rightfully deserve.
Sincerely - Elizabeth English Team Leader SWCNEP
Our motto Passion.... Persistence....Vision
The following are evaluation comments from students of the 2015 Kenyan SWCNEP
-Started empty on knowledge. Look at me now knowledgeable, confident and competent
-The Australian tutors were a blessing to us. Your effort will not be in vain.
-Clinical provided such exposure for me and it was awesome.
-Life changing course.
-It made an impact on me and I will transfer the impact to my country
-I am a better nurse now
-Tutors all brilliant and friendly. Very helpful. Has changed my whole perspective
-Grateful that whole team from Australia has been able to push through many obstacles to make sure the program went well
God bless you all
-I promise to continue practising the knowledge I have received.
-I didn’t know much about computers – now I can type my own assignments
-Improved my confidence in talking in front of people. – thanks to the oral presentations in class
-I am equipped with new knowledge now I need experience
-I have new friends from all over Kenya and Australia
-I have achieved more than I thought – came completely blank now have the knowledge that I would not have been able to get anywhere else.
-I have learnt such a lot
-Course really meaningful and very constructive
-I now know how to write an abstract, do a case study pictorial, power-point and present with ease.
-Now a full member of WCET and marketable to the world
-Have learnt innovation skills – to manage leaking wounds and fistula and can now deliver quality nursing care
-I can now deliver care not just in the ward but to the whole hospital
-The program is well organised and educative
-Did not think much about incontinence – now I need to take a different focus.
-I have achieved my objectives and can now mentor others with the knowledge I have gained.
-I am forever grateful for being given this chance. -God bless all the Australians
 2014 students practising with a doppler
2014 students practising with a doppler 2014 Team members presenting text book and doll with a stoma to Kijabe Hospital SWC Nurses Grace and Christine
2014 Team members presenting text book and doll with a stoma to Kijabe Hospital SWC Nurses Grace and Christine 2014 Graduation
2014 Graduation  2015 students hard at work in classroom
2015 students hard at work in classroom 2015 students discussing a patient at the bedside
2015 students discussing a patient at the bedside Wound care
Wound care.
 Crowded ward
Crowded ward
 Being loaded on to cattle truck after bus bogged on Kijabe road
Being loaded on to cattle truck after bus bogged on Kijabe road 2015 students
2015 studentsOrganizer
Trish Griffin
Organizer
Glen Forbes, VIC