Medical Expenses
Donation protected
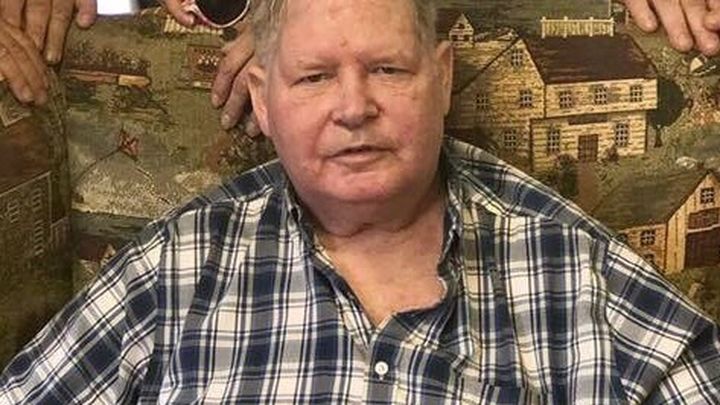
Anyone that knows Billy understands how big his heart is. He would drop everything in a second to be there for his friends and family. As many of you know, Billy's father became ill recently and has been hospitalized. Most recently, his father was transported to Cleveland, Ohio where his lung specialists are. While his father is receiving the best care possible, he continues to remain in critical condition. Billy and his family are staying in Cleveland and commuting back and forth to the hospital daily. The hotel, gas money, and food money are all expenses they did not anticipate. Friends, now it's our turn to show Billy how much we love him. Please consider donating to help ease the financial stress for Billy and his family so they can put their focus where it needs to be. If you are unable to donate, please say a prayer for Billy and his family while they are in the trenches of a very difficult time right now.
 Organizer and beneficiary
Organizer and beneficiary
Seth Fleetwood
Organizer
Bloomsburg, PA
William Welch, Jr
Beneficiary


