
Solve Alex's Medical Mystery
My name is Alex Haagaard, and I am a 29 year-old artist, writer and disability rights activist living in Ontario, Canada. I am asking for help to get some desperately needed answers about serious and unexplained medical symptoms that I've been dealing with for the past 25 years, with virtually no help from our healthcare system. This is my story:
My long and uncertain medical history
I began complaining of joint pain when I was four years old. I learned to tell left from right by remembering that my left knee was the one that always hurt. My doctors told me that it was just growing pains. A few years later, my right knee started hurting the same way - I told my doctors that it often felt like my kneecap had popped out of place. I'd collapse while climbing stairs, or trying to stand up out of a chair. Still growing pains, they said.
(My knees are very hypermobile, and have been prone to hyperextending and dislocating since I was four years old.)
Another thing that happened at age four was that our family doctor noticed my chest was covered in small purple bruises, about the size of pinheads, where I had been scratching some hives. They sent me to Sick Kids Hospital in Toronto where I was tested for everything from HIV to lupus to leukemia. All the tests came back negative. Eventually, I was 'diagnosed' with idiopathic thrombocytopenic purpura (ITP) - a disorder with no known cause, which results in low quantities of platelets, the cells that help your blood to clot. ITP usually happens in children, usually after exposure to a virus or medication, and it usually resolves quickly. I've had my low platelets for 25 years now. Interestingly, though, while my platelet counts have gone up and down over the years, my doctors have often emphasised to me that my counts are too high to cause spontaneous bleeding or bruising. They've never seemed very interested in explaining why it is that I experience both of these.

(The blue bruise on my breast is from my cat sitting on my chest. The brown bruise on my arm is from pinching my skin in a folding door. I'm not sure what caused the fading brown bruise on my knuckles, but I suspect it was the brace that I wear to prevent my wrist from dislocating when I use my wheelchair.
(I got this bruise from...lying on my side in bed?!)
(I...think I scratched a bug bite or something? I'm not sure. My arm felt wet and I looked over and here we are. This happens a lot.)
Over the years I've developed a number of other symptoms and conditions, including chronic migraines, severe stomach upset (i.e., having runny bowel movements three or four times a day), fainting spells, breathing difficulties, tinnitus, narcolepsy, neuropathic pain and tachycardia.
Whenever I've brought one of these to the attention of my doctors, the response has been to test me for a few common conditions (often the same things over and over again) then, when those tests come back negative, to either drop the issue entirely, or give me yet another idiopathic label and advice that amounts to "exercise more and suck it up". (The only exception here is my narcolepsy. That only took three years, three sleep specialists and two countries to get a correct diagnosis.)
Last year, in response to a blog post in which I detailed my experiences with chronic illness, I was contacted by a few people who suggested I look into the possibility that I might have a disorder called Ehlers-Danlos Syndrome, a hereditary connective tissue disorder. These people included a doctor who does advocacy work to improve the clinical diagnosis and treatment of this poorly recognised and widely misunderstood. My initial reaction to these suggestions was skepticism: from what little I knew of Ehlers-Danlos, its main feature was joint hypermobility, and I wasn't hypermobile, other than my knees.
But as I began to meet more and more people with Ehlers-Danlos online, and learned more and more about their experiences with the condition, I discovered that they matched many of my own experiences, to an almost surreal degree. I learned that Ehlers-Danlos tends to occur alongside a pair of conditions called Postural Orthostatic Tachycardia Syndroe (POTS) and Mast Cell Activation Syndrome (MCAS) which explained even more of my mysterious symptoms.
I also discovered that I was more hypermobile than I had initially realised.
(My hypermobile fingers)
After a few tries on my part, my GP agreed to refer me to the new Ehlers-Danlos clinic in Toronto.
When I broached the possibility that I might also have MCAS, she told me that there is no test for that, so I may as well just start on antihistamines and see if that helped at all. This isn't true; there is indeed a test for MCAS. But I felt that if I pushed the issue I'd be seen as 'test-seeking'. So, I began taking antihistamines - and this was the first major breakthrough I ever had in treating any of my symptoms. Specifically, when I started taking them, I hadn't had a solid bowel movement in about 15 years. I've now been taking large doses of antihistamines every day for about 10 months; my stools are nearly always normal, and I'm having them every one or two days, rather than three or four times each day.
After the pain specialist I'm seeing to manage my migraines became concerned about my heart rate (my resting heart rate hovers between 120 and 140), my GP also ordered a 48-hour Holter monitor - a device that continuously records your heart's activity. When the results of the test came back, she said, "Everything's normal. You have a few extra beats, and your heart rate went up to 180 a few times, but it looks like you wrote that that was when you stood up or were climbing stairs." And that was that.
I've dealt with a number of medical professionals over the past year who were horrified by my resting heart rate, until I told them it's always like that, at which point a few of them have even said, "Oh, that's alright then." No one has ever thought it might be worthwhile to have it diagnosed more specifically than, "it looks like you probably have some sort of dysautonomia."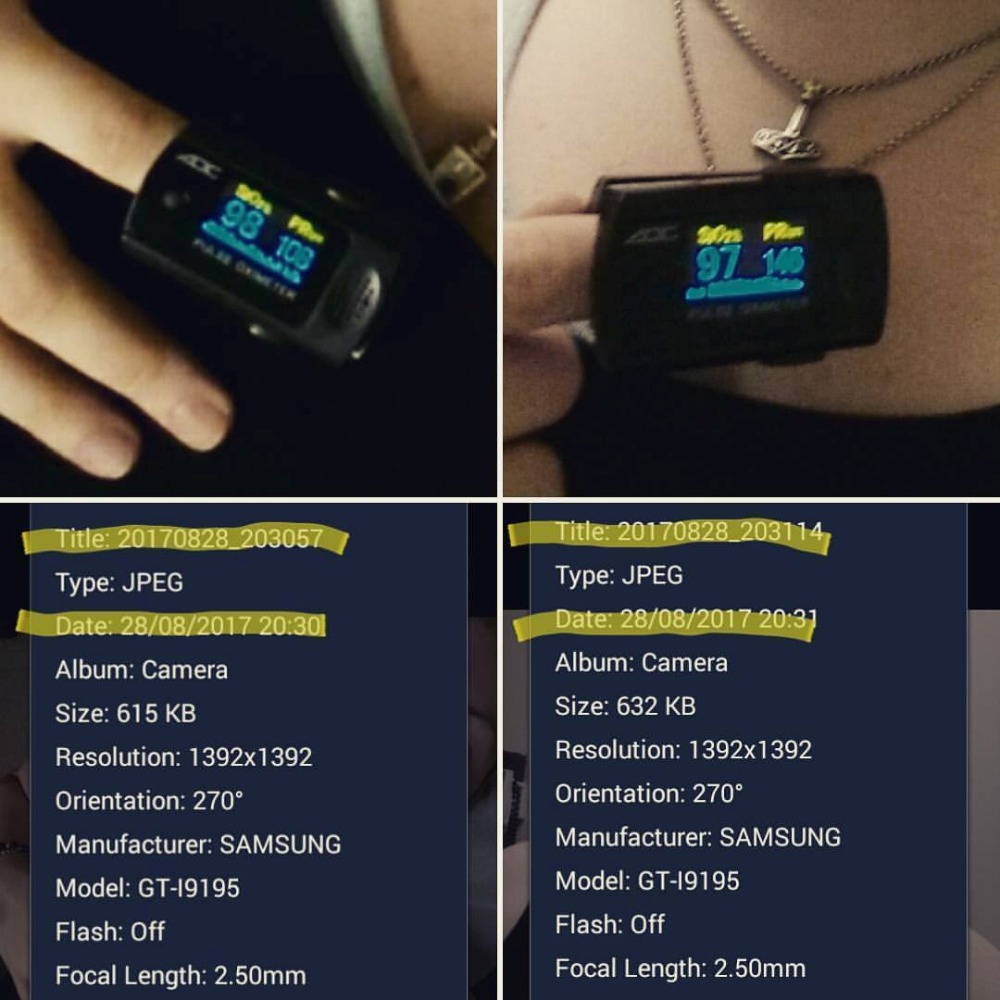
(My heart rate while lying down - 108bpm - versus 17 seconds later, after standing up - 146bpm. That probably means POTS. Of course "probably means" from a patient means literally nothing in a medical setting.)
Fast forward to this August, and my appointment with the Ehlers-Danlos clinic in Toronto. They emphasised repeatedly that they are using a set of new, stricter criteria for diagnosing Ehlers-Danlos, and that many people like me who feel the condition would explain their symptoms are disappointed when they don't fit the criteria. Their exam focused on the criteria for hypermobile Ehlers-Danlos, the most common subtype of the disorder. Sure enough, I wasn't hypermobile enough to fit the new criteria. They ignored the fact that under the new criteria, my fragile skin, which is ripped off in strips by bandages and kinesiology tape, rules me out for the hypermobile type anyway. When I explained that I more strongly suspect the vascular type of Ehlers-Danlos, they told me that because I've never had an organ rupture or an aortic dissection, and that because I don't know whether I have any family members who've experienced those events either, there is no reason to send me for genetic testing.
Now, here's the thing. Ten years ago, I spent a night lying on a gurney in my local ER, screaming in pain and shitting pints of blood. This was recorded as somatisation disorder, because I swore at the doctor when he berated me for screaming.
I know now that was probably a tear in my bowel that went undiagnosed. So were the other times I’ve had bloody stools over the past 10 years, that got shrugged off as constipation even as I explained I hadn’t had a solid bowel movement in 15 years.But because these were never diagnosed, they count for nothing in my medical history.
Similarly, there is no accommodation to be made for the fact that my familial medical history is woefully incomplete, because my mother came to Canada as a refugee at age five, and my father's family is both largely estranged, and not particularly well-versed in their own medical history (as might be expected, given that they grew up in a tiny, mid-century Danish farming village).
And so, apparently it is not worth testing me vascular Ehlers-Danlos - a condition that is most often diagnosed when someone dies from the organ rupture that would qualify them for genetic testing. Because, to be clear, organ ruptures and aortic dissections are highly fatal, particularly if they're not caught in a timely manner, which they're usually not.
This is why conclusive diagnosis of vascular Ehlers-Danlos is so important: it enables doctors to know that a patient complaining of chest or abdominal pain is likely experiencing a bowel perforation or an aortic dissection, and to treat them quickly, maximising their chances of survival. Conclusive diagnosis of vascular Ehlers-Danlos is very literally a matter of life and death.
It's worth noting that those strict new criteria
for diagnosing Ehlers-Danlos actually say in regard to the vascular subtype:
There are twelve minor criteria. Minimal clinical standards suggesting vEDS diagnostic studies should be performed are: a family history of the disorder, arterial rupture or dissection in individuals less than 40 years of age; unexplained sigmoid colon rupture: or spontaneous pneumothorax in the presence of other features consistent with vEDS. Testing for vEDS should also be considered in the presence of a combination of the other “minor” criteria. [emphasis mine]
(I have five, arguably six, of the minor criteria: easy bruising, hypermobility of small joints, history of muscle / tendon rupture, chronic joint subluxations / dislocations, gingival recession. I also have thin, translucent skin, but this is now substantially masked by the fact that I am fat.)
The doctor at the Ehlers-Danlos clinic told me that Canada has substantially tightened the criteria required to refer someone for genetic testing in the past ten years.
In my activism, I often talk about the flaws and inequalities within socialised healthcare systems, including our own. But I’ve always accepted the assumption that no one will ever die in Canada for lack of emergency medical care.
Now I realise that there will be a day, in the future, when I will once again find myself lying in an ER, screaming in pain while blood pours out of my bowel.
And I know that because I have no diagnosis, and because I am a woman, they will leave me screaming for hours.
And I know that maybe, this will be the time my bowel has finally perforated all the way through.
And that maybe, here in socialist Canada, I will die for lack of emergency care.
What am I asking for?
Vascular Ehlers-Danlos is usually diagnosed after someone has died from the organ rupture that would qualify them for genetic testing.
This is why conclusive diagnosis of vascular Ehlers-Danlos is so important: it lets doctors know that a patient complaining of chest or abdominal pain is likely experiencing a bowel perforation or an aortic dissection, and to treat them quickly, maximising their chances of survival. Conclusive diagnosis of vascular Ehlers-Danlos is very literally a matter of life and death.
I do not want to die a painful death for lack of a diagnostic label. Therefore, I am asking for you to help me finally, after 25 years, get some conclusive answers about what is happening inside my body.
I need:
1. An "Ehlers-Danlos Syndrome and related disorders" panel from LifeLabs. This will check me for a number of alleles (gene types) that have been associated with vascular Ehlers-Danlos.
2. An upright MRI in Kamloops, BC, to verify that I have a Chiari malformation. Chiari malformation occur when your brain starts to slip through the hole at the bottom of your skull. This creates problems with the pressures both in your skull and in your spine, and can produce a number of symptoms, including chronic headaches, tinnitues, sleep disorders, dysautonomia, nerve damage, and eventual paralysis. Chiari malformations can be a complication of Ehlers-Danlos.
I have a Chiari. It's visible on a normal MRI that I had two years ago while living in the UK, and a number of my friends who also have Chiari malformations agree - but the radiologist in the UK did not. The problem with Chiari, as with Ehlers-Danlos, is that most general radiologists are completely unfamiliar with what it looks like. Moreover, doctors here in Canada would be unlikely to accept a scan performed in the UK as valid diagnostic evidence. 
(An image from my 2016 supine MRI, which shows my Chiari malformation.)

(Then there was this weird looking thing, which I was told was an artefact, but to be entirely honest, I'd like to get that double-checked too...)
But in addition to my contested scan, I also have so many of the symptoms of a Chiari, including probable nerve damage: when the doctor at the Ehlers-Danlos clinic was testing my reflexes she just...couldn't get them. She had to hit my joints over and over, so hard it hurt, she made me look away, and pull on my finger to trick my brain. She kept having to tell me to pull harder and harder until I was a bit worried I was about to dislocate my finger. Finally, she was able to get a tiny response from each of my joints. She said this was normal, since everything was symmetrical. This is not remotely normal. It's a sign of nerve damage.
Because a Chiari malformation involves the brain slipping out through the bottom of the skull, they are most easily seen, and usually diagnosed, using upright MRIs, where the patient stands during the scan. The only privately available, upright MRI I have been able to locate within Canada is located in Kamloops, BC.
I would like:
3. A "Marfan, Loeys-Dietz Syndrome and related disorders" panel from LifeLabs. This will check me for a number of alleles (gene types) that have been associated with Marfan Syndrome and Loeys-Dietz Syndrome - two genetic disorders that have similar symptoms to vascular Ehlers-Danlos. This panel is of lower priority for me, because these two disorders do not seem to fit my symptoms as closely as vascular Ehlers-Danlos.
4. A normal MRI of my spine to check for syringomyelia, which is a common complication of Chiari malformations, a result of increased fluid pressure on the spinal cord. This is of lower priority for me, because my hope is that once the Chiari is diagnosed, doctors will be more willing to follow up on it.
What will your help mean?
You may be helping to save my life in an emergency. I can't prevent the breakdown of my body, but being able to get the care I need quickly will make a big difference in my health outcomes.
You will be helping me to access benefits to help me survive. Right now, I am receiving disability benefit from Ontario Works. I get $480 per month to cover room and board, and an additional $60 to cover any other expenses I may have. (To be clear, I spend $90 a month just on antihistamines.) I am living with my parents, in the hometown where I was severely bullied growing up, with no access to public transit, no license (since, you know, narcolepsy), and no job prospects. This is taking a severe toll on my mental health and I am frequently feeling suicidal. I have held off applying for the more substantial Ontario Disability Support Program because I know that with only one conclusive diagnosis (narcolepsy) - which is both rare and very poorly understood in terms of its disabling impact - I am unlikely to be approved, and I don't have the emotional or physical strength to go through an appeals process. I was desperately hoping that I would receive a conclusive diagnosis from the Ehlers-Danlos clinic that could support my ODSP application, but no such luck.
You will be helping me to access accommodations at work and school. If I am ever able to return to school or to work, my success will depend on being able to access accommodations related to my chronic pain and fatigue. Without a conclusive diagnosis, it is much harder - often impossible - to access accommodations.
You will be helping me to get treatment for my conditions. There are no cures for Ehlers-Danlos, or for Chiari malformations, but specialised care can help a great deal in managing symptoms. There are also surgeries that can help alleviate some of the symptoms of Chiari malformations. But to access any of this requires a conclusive diagnosis.
If you've read this far, thank you so much for your time. If you are able to donate, every little bit is much appreciated. If not, sharing is also a huge help!
And either way, most importantly, please know that I am far from the only person in Canada who is in desperate need of healthcare, but can't access it because of care rationing. Quebec recently played host to a medical conference who topic was "the problem of overdiagnosis", framed as a problem of health economics and sustainability. But the problem is really that we frame people's lives in terms of economics. Spend some time with the disability and chronic illness communities on Twitter, and you will see an incredible amount of suffering caused by the treatment of healthcare as an economic problem, and the handling of disabled lives as economic burdens - including within vaunted socialised healthcare systems such as those here in Canada and in the United Kingdom. Stop comparing our system favourably to the United States, and consider writing your MP and MPP to advocate for more inclusive healthcare policy.


