Trayson's Battle with Sickle Cell
Donation protected
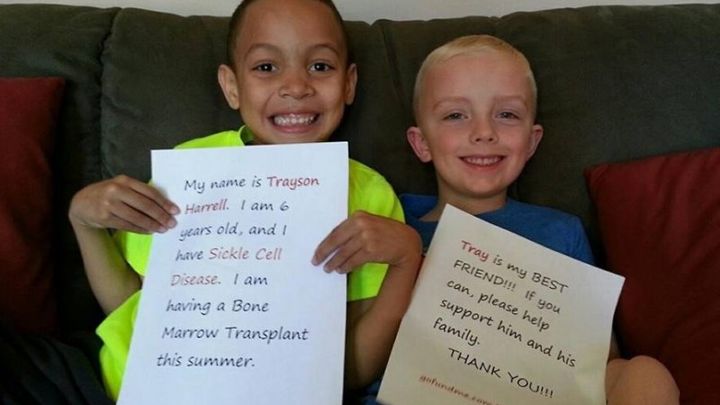
Trayson Eric Harrell: Sickle Cell Warrior
Trayson Harrell was born on December 9, 2008 to parents, Eric and Amy, in Great Falls, Montana. He came one week earlier than expected. Truth be told, I was able to choose his birthday because little Trayson wasn’t so little. Trayson weighed in at a healthy 10 pounds 11 ounces and looked like a defensive lineman in the making. He even lifted up his head in the delivery room shortly after the planned delivery! We were so excited to finally meet our Big Boy Trayson!
Trayson and I were feeling great and heading home after a few days in the hospital. Daddy was as proud as ever of both the new mama and his new bundle of joy, Trayson, to whom we called “Tray” from the beginning. We had been adjusting to life with Trayson and having nice visits from friends and relatives to meet the new guy in town.
On December 19, 2008, we were visiting Gramma and Papa, the Veltkamps. My phone rang, and I noticed it was the clinic calling, which seemed odd on a Friday so late in the afternoon. It was our pediatrician calling to let me know information about Trayson’s newborn blood work, like a 10 day report? This phone call was the worst moment of my life, although I didn’t realize it at the time. Trayson’s blood work was showing a genetic blood disorder called Sickle Cell Disease (SCD). I explained to the doctor that I wasn’t sure how this was possible but admitted that I didn’t really know what it all meant. I had heard of SCD but never took any effort to research it for any purpose. I also explained that we knew Eric carried the sickle cell trait because he found out when he was in the military. The pediatrician immediately asked if I had been checked for the trait as well. I tried to explain that I was not sure when or where I would have been checked. I think she could hear the dismay in my voice, and she invited us to come to the clinic and have some blood work done to confirm what they were seeing in the labs.
Sickle cell trait is widely carried in African Americans but not as widely in Caucasians. Some percentages I came across said 60+% in African Americans and less than .20% in Caucasians such as myself. In order to be born with SCD, both parents must pass on the recessive trait. We were hoping for an error in the lab or just mistaken blood work. After I had my blood drawn and analyzed, it was determined that I, too, had sickle cell trait. Could Eric and I have both passed on the recessive trait to Trayson? After drawing Trayson’s blood again to double and triple check the results, our 10 day old baby boy, Trayson, was confirmed to have Sickle Cell Disease-SS. This news was a huge blow to the family. It changed our lives forever.
Sickle Cell Disease is a blood disorder in which the bone marrow in the body makes misshapen blood cells, “sickle shaped” cells. These misshapen cells tend to stick together and don’t flow through vessels like the round “normal” blood cells. This sludgy blood flow can cause blockage of vessels which can cause severe pain crises or even lead to a stroke. This lack of fluidity also affects the oxygen saturation of the body because the cells are not efficiently carrying oxygen to the vital organs which can lead to organ damage. These abnormally shaped blood cells die every couple of weeks which requires the body to work harder to continually make more blood cells. A normal blood cell can live for months. The disease itself is very complicated, and some people have severe problems while others can have mild to no symptoms. There are lots of resources available to learn more about SCD-SS.
After hearing the diagnosis, our minds were spinning. We definitely needed to do our research and hoped to understand better what we were about to face with Trayson. We were hopeful he was going to have mild symptoms but were ready to face a fight. We just didn’t know exactly what we were getting into nor were we prepared for this fight. It has been a tremendous learning experience and the fight of our lives, especially for young Tray.
Tray was a very calm and relaxed baby, and if we didn’t know better, we would have thought there was absolutely nothing wrong with him. On the outside, he looked as normal as can be. The first year of his life was full of happy times with very little to report except for a few visits to the Emergency Room for low grade fevers of 101 or higher. There are certain things that send us to the ER no matter what, and fever was the number one problem we faced in his first year. We were linked in with a hematologist here in Great Falls, but there was not a local pediatric hematologist available to us. We had a few visits to the hematologist who informed us that at some point we would need to go to a sickle cell center to be evaluated and have a special brain scan called a TCD, Transcranial Doppler, to measure his risk for stroke. The hematologist worked closely with our regular pediatrician and advised us to schedule something with a center sometime between the ages of two and four years depending on his health.
About two weeks after Trayson’s first birthday, he was hospitalized for what was diagnosed as RSV, a respiratory illness often in young children. This was a painful and frightening time for us because we knew he already had issues with oxygen levels. We had our first respiratory illness which kept us hospitalized for about five days, the longest and most traumatic thus far. The diagnosis actually had nothing to do with Sickle Cell Disease, but the SCD did complicate the matter and made it more difficult to recover. Plus, Trayson did not take too kindly to having blood drawn which later became known as “a bonk” to all of us. From here, he grew very familiar with “bonks” unfortunately.
The next two years, 2010 and 2011, were filled with times of heartache and confusion as well as learning about SCD as we went. In April of 2010, we went through our first pain crisis with Trayson. At the time, we were unaware of what could have caused it and really baffled by how suddenly it came on and seemingly out of nowhere. Now I know he was dehydrated which is a leading cause of pain crisis in SCD, but at that time, we just weren’t educated fully. In these two years, we averaged approximately 3-4 hospitalizations and 2-3 blood transfusions each year not to mention the numerous visits to the ER, which usually ended with an admission to pediatrics or a long night of tests, antibiotics, and blood work (lots of bonks). Most of the problems came from common illnesses that were complicated by the low oxygen saturation due to SCD. Every hospitalization, bonk, ER visit, and illness was excruciating for all of us.
We began to understand how serious this disease was and what it was doing to Trayson whether he was healthy or ill. We also now recognized that no matter what he looked like on the outside, his insides were really working hard and fighting a battle every day. We were still seeing the hematologist in town and making some plans to figure out where to go from here. He was adamant, along with our pediatrician, about us heading to a center sometime in the near future. Thus came the year 2012. This year was seemingly shaping up to be very similar to the previous couple of years but magnified even more with recurring issues due to oxygen levels, fevers, and pain crises. There were times when Trayson was in so much pain, he was inconsolable. We tried all kinds of different pain relievers including using narcotics for pain at home and morphine through an IV in the hospital…for a three year old! It was in the fall of 2012, I decided we needed to take some further action since his issues were mounting, and it seemed he may have a severe rather than mild form of this disease. I started searching around some children’s hospital websites located near our area. The closest sickle cell specialists were in Washington State and Colorado. I found the name of a social worker who worked with the Children’s Hospital of Colorado located in Aurora, CO. My oldest brother and his family still had a home in Colorado Springs, so I thought it would be a good choice in case it would help to have some family nearby especially if multiple trips to Colorado would be required. We made an appointment to be seen by a hematologist at Children’s Hospital of Colorado in October of 2012, when Trayson was two months from being four years old. We would also have the noteworthy Transcranial Doppler (TCD) we had been informed about earlier on in his plan of care.
Our initial visit to the hospital in CO yielded a wealth of information and more specific information to Trayson’s version of the disease. They were impressed with how big and healthy he was for having SCD. Often times, kids with SCD appear to be small and sometimes frail. The examination and consultation with the hematologist was extremely informative and alarming at the same time. We were unaware of some things we really needed to pay more attention to such as the amount of water and calories needed each day for kids with SCD. There were many other things we didn’t know such as not using ice packs, trouble with temperature extremes, swimming issues, contact with reptiles, and cold weather problems. We could think back to some of our previous episodes and attribute them to these new and very specific things we were learning for the first time. It was surprising to learn that Trayson’s water requirement is 64 ounces a day, and he needs twice as many food calories as a normal child. The doctors assured us we were doing “something” right because other than the SCD, he seemed very healthy. They have even described him as one of the healthier looking kids they had seen living with SCD. At this visit, we were able to have his blood hyper-matched so that future blood transfusions would be better matched to Trayson’s blood since he has to have repeated transfusions. After several blood transfusions, your body starts to build up antigens, and the hyper-matching would avoid this as much as possible. We did receive some discouraging news from this initial visit. The Transcranial Doppler, the brain scan measuring velocity of blood flow to the brain, resulted in a “high-conditional” reading on one side which meant he had a high risk for stroke. This news was difficult to swallow because we had such positive thoughts regarding the brain scan. It was disappointing news but required immediate attention with no time to dwell. At this point for medications, Tray had been consistently on Penicillin as a preventative measure along with the different types of pain medication we had to try during each pain crisis. With the new findings, we would now add an additional medication called Hydroxyurea, a type of chemotherapy that would increase the amount of fetal hemoglobin. This medication would support the blood flow in his body because there would be less of the SS hemoglobin. Hemoglobin is a protein in the red blood cell that carries oxygen. Low hemoglobin is common and a major factor in SCD. The new medication was supposed to help with the stroke risk as well as decrease the number of pain episodes, instances of hospitalizations, and decrease the chance of Acute Chest Syndrome (a possibly fatal respiratory illness in SCD). Hydroxyurea is also said to raise his hemoglobin up at least 1.0. Low hemoglobin contributes to the fatigue and low oxygen saturation. We came away from our first consult with a blood specialist knowing a whole lot more, paying attention to every little detail, hyper-matched blood typing, and a new medication to add to the medical management of SCD. We were due to see our Colorado doctor and have a repeat TCD in six months to see if there was going to be any improvement in blood flow to the brain. We were scheduled to return to Children’s Hospital of CO in March of 2013.
After we returned home from our first Colorado medical visit, we came home to various pain episodes as well as entered respiratory season which always seemed to affect Trayson. In early January 2013, shortly after the New Year, Trayson fell ill while at Gramma’s house. I was at work, and Eric was working out of town. Tray’s temperature spiked to over 103 degrees, and we were definitely headed to the clinic while calling his pediatrician and knew we would most likely be admitted to the hospital until they could determine what was causing the high fever. We spent about four days in the local hospital, and Trayson was not getting better. He was deteriorating when we thought he should be getting better. The local doctors thought it would be best to consult with Children’s Hospital of CO. The Great Falls and Colorado doctors together decided after the usual tests, labs, and chest x-rays, he had developed Acute Chest Syndrome (ACS) and would need to be airlifted to Colorado to better deal with the disease. ACS can be fatal if not treated quickly. The news of the airlifting was especially devastating because Eric had not made it home from working out of town in Miles City, and we would fly before he could get back to us to say goodbye. Trayson, of course, was scared and wanted his daddy there by his side. It would be the next day before Daddy could finally be with us. While in the hospital in Colorado, we learned more about ACS and endured many, many bonks with Trayson including another blood transfusion. It took seven “roller coaster” days at Children’s Hospital Colorado for Trayson to be able to come back home to Great Falls. Our total hospital stay in January of 2013 was 11 days. Due to the recent blood transfusion, we had to push back our next TCD appointment another three months in order to get a proper reading. In March of 2013, we were back in the hospital in Great Falls needing another transfusion. This caused the TCD to be pushed into the summer time, most likely in July. Our July 2013 visit to Colorado yielded a great result from the TCD. It seemed the Hydroxyurea had helped with the velocity of blood flow to his brain, and it was now in acceptable levels for SCD. This was great news for us and relieved all of the family, just a little. We did not let our guard down though and stayed vigilant in Trayson’s care. We would be making trips to Colorado every three months now to see Tray’s doctors there. The fall of 2013 seemed to go pretty smoothly as long as we were staying focused and following doctor’s orders with hydration, calories, rest, medications, regular checkups and blood counts. In October of 2013, we were linked in with a new pediatric hematologist closer to our home but still located 3 ½ hours away in Billings, MT. We were able to see her every six months as well, so we could limit our trips to Colorado to every six months. This way Trayson could be seen by specialists consistently every three months. While seeing our hematologist in Billings, we were able to connect with a pediatric pulmonologist (lung doctor) as well.
Although the fall was a pretty healthy time, Trayson fell ill on Christmas Day of 2013. He had a high fever, and we took him to the ER to go through the gamut of x-rays, tests, blood counts, and IV antibiotics or antibiotic shots in the thighs. We were admitted just for an overnight stay (which was rare) and sent home after tests showed he had Para Influenza II. We kept him very secluded and rested over the next few days and thought we had him better. It was New Year’s Eve of 2013, and we had canceled our company for New Year’s due to what we deemed a setback in Tray’s health. He just didn’t seem quite right. After years of dealing with these issues, our instincts kicked in, and we knew something was wrong. We took him to the ER and ended up with an admission to the hospital for Para Influenza again. This hospital stay did not go as well. Trayson deteriorated quickly (common for SCD), and his Para Influenza turned into another bout with ACS. After two days in the local hospital, they were planning to airlift us to Colorado for our second January in a row. Once we made the decision to fly, it took several more hours before takeoff due to weather and night flying. We arrived in Colorado in the wee hours of the morning. When we arrived, Trayson had deteriorated so much that he needed to be moved to Pediatric Intensive Care (PICU) immediately and put on a Bi-Pap machine to help him breathe. When we left Great Falls, he was requiring two liters of oxygen, but when we arrived, he was up to five liters of oxygen and struggling to breathe. The doctors asked me how long he had been that way, but it had only been a few hours since we left Great Falls. He had just gone downhill so fast, and it was frightening. We spent a few days in PICU on Bi-Pap and were able to move up to the hematology floor. He seemed to be getting better each day and of course this is why they released us from PICU. The next night after being moved from PICU, Trayson had a fit of coughing. He couldn’t stop coughing which caused him to cry. This coughing and crying was heartbreaking because we could not do anything to console him. As a parent, all we wanted was to take his pain away. The coughing and crying continued through all of our comforting, and this alerted our nurse. She came in to see what was going on and listen to his lungs but found him to be struggling to breathe. Then, suddenly, Trayson stopped breathing while Eric and I helplessly looked on. The nurse was quick to react and had a Code Blue going within seconds. Teams of doctors and nurses came in with some working on Trayson and others trying to console us. From my perspective, I could only stare at Trayson and will him to fight through this and come back to us. Trayson is such a fighter. He was able to regain his breathing again. We were immediately transferred back to PICU to go back on Bi-Pap until we figured out what was going on. Trayson was able to tell me later that day that he was having pain in his chest and abdomen which no one including doctors knew about. Trayson said he thought if he said he wasn’t having any pain, he would get to go back home. The pain he was having was causing him to take short, shallow breaths rather than the deep breaths required to clear his lungs. We immediately started him on round the clock morphine to alleviate this pain so he could breathe correctly to start healing. After two days in the PICU again, we were moved back to the hematology floor where we stayed for several more days to make sure he was out of the woods. Total hospital stay between Great Falls and Colorado was 14 days this time with most of it at Children’s of CO. After returning home, we felt like we had been in some crazy nightmare, but we learned a lot about Trayson, the patient. We began taking abdominal pain and chest pain even more seriously since they affected his breathing so much this go round. We were also able to get a pain medication, Dilaudid, which actually works for his severe pain. We keep this medication filled all the time in case we need something strong to battle the pain. Now, Trayson is very good about declaring pain and able to put it on a pain scale of 1-10. He knows anything above a five will need Ibuprofen and possibly Dilaudid. If he rates pain at seven or higher, we will treat with Dilaudid first thing to stay on top of the pain so it doesn’t affect his breathing. His arms and legs suffer pain as well, but these areas don’t affect the way he breathes as much and are easier to manage from home with pain meds. After this second airlifting, we continued with our follow up appointments to Billings later on in January 2014. We were scheduled to be back in Colorado for appointments the following April.
Before April came, Trayson was admitted to the hospital in March of 2014 for a respiratory illness. They found some infiltrates on his chest x-ray. This would be his 3rd bout with ACS although this occurrence didn’t require airlifting to Denver. We were able to get through the crisis here in Great Falls but knowing we would be in for some tough decision-making going forward. SCD has always required a lot of decision-making. I just knew we were on the brink of more decisions regarding Tray’s life. Three bouts of ACS by age five are quite a few for SCD and can cause lung damage as well as death. As we had seen, it causes the body to deteriorate quickly from bad to worse in very short intervals of time. We were currently looking at the possibility of lung damage.
At our April 2014 appointment in Colorado, we and the doctors decided to explore the option of a bone marrow transplant (BMT). The first step in exploring BMT is to swab all three of us to see if Eric and I happen to match. Then, the search for DNA matches for Trayson began. The doctors told us it would take about six weeks to find out if he has a match out there. My hopes were very high at first, but then I started looking into the matching process. My hopes began to diminish because it seemed so out of reach to have unrelated matched DNA. In late May of 2014, we were informed that Trayson actually has thousands of matches out there. These are gold standard 10 of 10 matches, and he has lots of gold standard cord blood matches as well. This was fantastic news for us. We were excited to explore the option of BMT!
In June of 2014, we were informed that Trayson would be nominated for a Make a Wish Foundation wish. Anything he would like to wish for could possibly be granted if he was selected. We did receive word about mid-summer that Trayson was actually selected, and the process would be started to grant his wish. His wish…he wants to meet Mickey Mouse and Darth Vader!!! Perfect! His wish is due to come true on May 26, 2015!!! Our local high school, Great Falls High School Bison, was able to sponsor Trayson for the whole wish! Great Falls High School has been very kind to us and supported Trayson in countless ways through fundraising and raising awareness about SCD. We are forever indebted to the students, staff, and administration at GFHS.
We all knew July of 2014 was going to be a busy month for Trayson. He even knew he would be busy traveling to both Billings and Colorado and could tell everyone how many days he would stay in a motel (loves motels!). In the middle of July, we were heading to Billings to have a sleep study along with our regular visit to our two specialists there. The pulmonologist ordered the sleep study which measures almost everything under the sun it seems. Trayson was quite a trooper with about 50 wires coming out of him! We later were informed of the sleep study results, and once again, there was good news and bad news. The good news was great news, but the bad news certainly overshadowed anything else. They discovered his oxygen saturation to dip into the 80s for 72% of the night. His average oxygen saturation over the 7.5 hours of sleep was 88%. This would not be positive news for his young organs. This is information I wished I had received earlier. These results would yield more medical management from home. Trayson would have to begin sleeping with oxygen every night. We would start immediately at ½ a liter and see how it goes. Eventually, we did move down to a ¼ liter, but Trayson does not enjoy sleeping with oxygen every night. He often asks how long he will have to wear the oxygen. It is a very hard question to answer. In addition to the oxygen at night, the pulmonologist recommended we start on an asthma regiment recommended by colleagues in Georgia. Tray was to begin taking another oral medication in addition to an inhaler twice a day. Since August of 2014, Trayson takes an inhaler, one pill and a vitamin in the morning, and he takes four pills and the inhaler in the evening along with the required oxygen at night. It seems like a lot of medication for a now six year old, but this is how we are supposed to medically manage SCD.
We would piggy back the July 2014 Billings appointment with another trip to Colorado for a Bone Marrow Transplant consult with an assigned transplant doctor at Children’s. Since we were fortunate to have some quality bone marrow matches for Trayson, we just had to explore our options. Knowledge is power. There we sat; the three of us, going through an exam of Tray and listening to a doctor explain BMT to us. Trayson was in the room, but he was busy playing so paid no attention to what we were doing. My sister-in-law, Kristen, was nice enough to videoconference into the consult, so we could have an extra set of ears and questions. The pros and cons of BMT are aplenty and were explained in great detail. We filtered through the science of it all and were left feeling extremely overwhelmed by the whole experience. It is hard to put into words, but I will try. Trayson has a very severe case of Sickle Cell Disease. The only known cure for this disease is bone marrow transplant. There are no guarantees. There will be complications. He will have chemotherapy for 7-10 days to wipe out all of his bone marrow including his immune system. Chemotherapy will be very difficult, and he will be very sick. He will lose his hair and have various side effects ranging from mild to severe. There is a high risk of graft vs. host disease (GVHD) where his body fights back against the new marrow. He will be hospitalized for anywhere from 4-6 months and will not be able to go back to school for a year. The ultimate risk is death. These words haunt me to this day. These are the words that create fear for this decision; however, BMT is the only known cure for SCD. Needless to say, we left the consult full of tough emotions and tough decisions. Trayson left the consult and couldn’t wait to get back to the motel (loves motels!). He was oblivious to the current news, and we let him be for now. Eric and I decided to make the rest of the Colorado trip enjoyable for Trayson and keep our emotions at bay until we returned home.
After returning home, my sister–in-law that was listening in to our consult invited us to come to North Carolina for a visit to the BMT doctors in their area. We were lucky to have this opportunity for a second opinion regarding BMT. In August of 2014, Tray and I flew to North Carolina to consult with doctors there. This visit was eerily similar to the first consult, meaning the second opinion was the same as the first. The only difference…I had to process this time without Eric since he stayed back in Great Falls to work. I felt as if this consult was a good confirmation of what may need to happen for Trayson’s sake.
At this point, returning from North Carolina, Eric and I really needed to sit down and talk about the decision facing us…whether or not to go forward with the BMT. This is the point in time we began the new medications to try to ward off any respiratory illnesses before they hit to avoid another ACS. It seemed a lot had transpired in the summer of 2014 where Trayson’s health was concerned. Shortly after returning from NC, Kristen set up a phone conference with a doctor in Cincinnati who was kind enough to chat with me about Hydroxyurea. This doctor is an expert on this drug we had been giving Trayson since 2012, but more noteworthy, he is not a transplant doctor. It was nice to hear the “other side” of the story from a doctor who believed in the medical management and living with SCD. He made a lot of sense to me and also asked me if we had “tried everything” before deciding to go to transplant. After discussing this information with Eric, we felt like we needed to give the new oxygen treatment and asthma medications an honest chance.
Trayson was due to start kindergarten at Lincoln Elementary, where I also teach, in September of 2014. He was indifferent about starting kindergarten, but after meeting his teacher, he felt a lot better about beginning the school year. School would be challenging in Montana due to the weather extremes, mostly cold weather issues which would most likely affect Trayson socially due to not being able to participate in outdoor activities such as recess. He is required to stay inside if the temperature dips below 50 degrees, if it is snowing, or there are extremely windy conditions. There are several other issues with SCD that could impact his schooling as well, so we immediately put an educational plan, a 504, in place to make sure he would get the services he needs academically in case of any complications that could arise. We already knew there would be several absences over the course of the year because of the various illnesses. We made sure the Lincoln staff was informed of his unique situation. The staff at Lincoln has been accommodating Trayson every step of the way. They have always been a huge support to our family, including emotional, physical, and financial support. We couldn’t have asked for a better situation for Trayson’s educational experience. He quickly made lots of new and fantastic friends. School really opened his eyes to the differences among him and his classmates. Starting school made Trayson realize how different he is from other kids, and how much he wants to be a normal child like his friends in class. Despite being around lots of other kids at school, he seemed to be staying pretty healthy through the fall of 2014. This was quite promising to us, and we attributed the good health to the addition of oxygen at night and the new asthma medications we were trying. We were hopeful that things would continue on smoothly from here.
In October of 2014, we traveled to Billings for our regular appointments and informed our hematologist that we would be “tabling” our discussion regarding transplant for now and would see how Tray does through the winter months and respiratory season with these new things we were trying. The conversation with both the hematologist and pulmonologist went very well, and they were supportive of our thinking at the time. From our perspective, we were having a hard time taking our seemingly healthy little boy and making him very sick and possibly ending in death. To us, the risk outweighed the reward at this point. These things haunted us, plus with these new medications and oxygen, it only seemed right to try everything possible before making a decision that could potentially end our son’s life. The decision was officially made, and a weight was lifted off of us. Now, we will do our best to keep Trayson healthy through the dreaded month of January and the rest of the respiratory season.
Unfortunately, when we returned home from Billings in October of 2014, Trayson fell ill. This illness caused Tray to miss out on trick or treating on Halloween, but a few nice friends of ours allowed us to “make up” Halloween the following weekend. We were not hospitalized, but this illness did cause his hemoglobin to drop below 7.0 and required a transfusion along with several missed school days. He bounced back from this illness after having the transfusion, resting up, and supplementing with oxygen at home to keep him above 95%. His health improved, and he was back into the swing of things at school.
Trayson turned six years old on Dec. 9, 2014, and he seemed to be doing very well after the setback in October. He was looking forward to Christmas, but we as parents, were not without worry. This is the time of year Trayson struggles the most with his health. When we had a two week break from school, we kept him in a “bubble” at home all but about two days. We felt we could protect him from the illnesses that were out there during this rough time of year. We were successful in keeping him healthy through December and most of January and were very excited at the possibility of staying relatively healthy throughout respiratory season.
In the latter part of January 2015, Tray did fall ill with a high fever which was treated by the clinic with strong antibiotics and sent home to manage with oxygen, rest, and medicine. We were happy to be able to manage this illness at home which seemed easier with oxygen at our fingertips. When February came around, we felt as if he was better but decided to hold him out from school an extra day and the weekend. By then, he surely would be well enough to go back to school. During this illness, we were having his blood counts checked often to make sure his hemoglobin stayed above 7.0 as well as a chest x-ray to make sure his lungs were staying clear. After the weekend, Eric took him in for blood counts, and his hemoglobin had dropped a bit. We were scheduled to have a blood transfusion after this drop in hemoglobin, but he wasn’t having too many symptoms of illness. The next day, he woke up coughing on the day of the scheduled transfusion. The pediatrician suggested another chest x-ray before the transfusion, and our routine blood transfusion to boost hemoglobin turned into a full blown hospitalization. The chest x-ray showed infiltrates in his right lung that were not there two days prior. The blood transfusion went fine, but our worries shifted to Trayson’s next bout with ACS. This would be his fourth instance of Acute Chest Syndrome. This time his fever spiked, and he went from seeming fine to being very, very ill. This one came on very suddenly and didn’t waste any time. Colorado doctors consulted with our doctors here and decided immediately to airlift to Children’s Hospital for our third time. This was a confusing time for Trayson because he even recognized himself getting better and then suddenly worse. We arrived in Colorado to the teams of doctors and nurses we had come to know over the last few years. This time, we made it before Trayson was in dire need. Quick decision-making and experience with SCD and ACS made this hospital stay shorter, but this visit was an eye opener for both Eric and me. We spent seven days in the hospital and were reintroduced to the BMT doctor and had a very candid conversation about Trayson and his future with SCD. We returned from Colorado knowing the conversation about BMT was back on the table, and now our decision time was limited. We would need to let the BMT team know our decision by the end of February 2015 to have enough time to find a donor, harvest marrow, and be ready for a summer transplant.
Eric and I spent a great deal of time weighing our options. It was clear that medical management of SCD may not be working for our son. At any point, on any day, Trayson could be taken from us because of this disease. It is a very real experience. At the end of February 2015, I made the call to the BMT team at Children’s Hospital of Colorado to set up his first appointment on June 16, 2015. We all will be in the fight of our lives to save Trayson’s life. We will never feel comfortable, but we feel confident we have made the right decision for Trayson.
For the time being, Trayson is receiving chronic blood transfusions every other week to keep him as healthy as possible leading up to transplant. These blood transfusions are a huge time commitment, but Trayson is adapting as well as he always does to adversity.
Every day, Trayson fights an internal battle we know nothing about. Sickle Cell Disease is a horrific battle and often results in short life expectancy or poor quality of life. Everyone living with the disease goes through different experiences and complications. Trayson is our hero, and we love him more than anything in the world. He is nothing less than a SICKLE CELL WARRIOR, and WE WILL FIGHT this battle together no matter what.
Trayson Harrell was born on December 9, 2008 to parents, Eric and Amy, in Great Falls, Montana. He came one week earlier than expected. Truth be told, I was able to choose his birthday because little Trayson wasn’t so little. Trayson weighed in at a healthy 10 pounds 11 ounces and looked like a defensive lineman in the making. He even lifted up his head in the delivery room shortly after the planned delivery! We were so excited to finally meet our Big Boy Trayson!
Trayson and I were feeling great and heading home after a few days in the hospital. Daddy was as proud as ever of both the new mama and his new bundle of joy, Trayson, to whom we called “Tray” from the beginning. We had been adjusting to life with Trayson and having nice visits from friends and relatives to meet the new guy in town.
On December 19, 2008, we were visiting Gramma and Papa, the Veltkamps. My phone rang, and I noticed it was the clinic calling, which seemed odd on a Friday so late in the afternoon. It was our pediatrician calling to let me know information about Trayson’s newborn blood work, like a 10 day report? This phone call was the worst moment of my life, although I didn’t realize it at the time. Trayson’s blood work was showing a genetic blood disorder called Sickle Cell Disease (SCD). I explained to the doctor that I wasn’t sure how this was possible but admitted that I didn’t really know what it all meant. I had heard of SCD but never took any effort to research it for any purpose. I also explained that we knew Eric carried the sickle cell trait because he found out when he was in the military. The pediatrician immediately asked if I had been checked for the trait as well. I tried to explain that I was not sure when or where I would have been checked. I think she could hear the dismay in my voice, and she invited us to come to the clinic and have some blood work done to confirm what they were seeing in the labs.
Sickle cell trait is widely carried in African Americans but not as widely in Caucasians. Some percentages I came across said 60+% in African Americans and less than .20% in Caucasians such as myself. In order to be born with SCD, both parents must pass on the recessive trait. We were hoping for an error in the lab or just mistaken blood work. After I had my blood drawn and analyzed, it was determined that I, too, had sickle cell trait. Could Eric and I have both passed on the recessive trait to Trayson? After drawing Trayson’s blood again to double and triple check the results, our 10 day old baby boy, Trayson, was confirmed to have Sickle Cell Disease-SS. This news was a huge blow to the family. It changed our lives forever.
Sickle Cell Disease is a blood disorder in which the bone marrow in the body makes misshapen blood cells, “sickle shaped” cells. These misshapen cells tend to stick together and don’t flow through vessels like the round “normal” blood cells. This sludgy blood flow can cause blockage of vessels which can cause severe pain crises or even lead to a stroke. This lack of fluidity also affects the oxygen saturation of the body because the cells are not efficiently carrying oxygen to the vital organs which can lead to organ damage. These abnormally shaped blood cells die every couple of weeks which requires the body to work harder to continually make more blood cells. A normal blood cell can live for months. The disease itself is very complicated, and some people have severe problems while others can have mild to no symptoms. There are lots of resources available to learn more about SCD-SS.
After hearing the diagnosis, our minds were spinning. We definitely needed to do our research and hoped to understand better what we were about to face with Trayson. We were hopeful he was going to have mild symptoms but were ready to face a fight. We just didn’t know exactly what we were getting into nor were we prepared for this fight. It has been a tremendous learning experience and the fight of our lives, especially for young Tray.
Tray was a very calm and relaxed baby, and if we didn’t know better, we would have thought there was absolutely nothing wrong with him. On the outside, he looked as normal as can be. The first year of his life was full of happy times with very little to report except for a few visits to the Emergency Room for low grade fevers of 101 or higher. There are certain things that send us to the ER no matter what, and fever was the number one problem we faced in his first year. We were linked in with a hematologist here in Great Falls, but there was not a local pediatric hematologist available to us. We had a few visits to the hematologist who informed us that at some point we would need to go to a sickle cell center to be evaluated and have a special brain scan called a TCD, Transcranial Doppler, to measure his risk for stroke. The hematologist worked closely with our regular pediatrician and advised us to schedule something with a center sometime between the ages of two and four years depending on his health.
About two weeks after Trayson’s first birthday, he was hospitalized for what was diagnosed as RSV, a respiratory illness often in young children. This was a painful and frightening time for us because we knew he already had issues with oxygen levels. We had our first respiratory illness which kept us hospitalized for about five days, the longest and most traumatic thus far. The diagnosis actually had nothing to do with Sickle Cell Disease, but the SCD did complicate the matter and made it more difficult to recover. Plus, Trayson did not take too kindly to having blood drawn which later became known as “a bonk” to all of us. From here, he grew very familiar with “bonks” unfortunately.
The next two years, 2010 and 2011, were filled with times of heartache and confusion as well as learning about SCD as we went. In April of 2010, we went through our first pain crisis with Trayson. At the time, we were unaware of what could have caused it and really baffled by how suddenly it came on and seemingly out of nowhere. Now I know he was dehydrated which is a leading cause of pain crisis in SCD, but at that time, we just weren’t educated fully. In these two years, we averaged approximately 3-4 hospitalizations and 2-3 blood transfusions each year not to mention the numerous visits to the ER, which usually ended with an admission to pediatrics or a long night of tests, antibiotics, and blood work (lots of bonks). Most of the problems came from common illnesses that were complicated by the low oxygen saturation due to SCD. Every hospitalization, bonk, ER visit, and illness was excruciating for all of us.
We began to understand how serious this disease was and what it was doing to Trayson whether he was healthy or ill. We also now recognized that no matter what he looked like on the outside, his insides were really working hard and fighting a battle every day. We were still seeing the hematologist in town and making some plans to figure out where to go from here. He was adamant, along with our pediatrician, about us heading to a center sometime in the near future. Thus came the year 2012. This year was seemingly shaping up to be very similar to the previous couple of years but magnified even more with recurring issues due to oxygen levels, fevers, and pain crises. There were times when Trayson was in so much pain, he was inconsolable. We tried all kinds of different pain relievers including using narcotics for pain at home and morphine through an IV in the hospital…for a three year old! It was in the fall of 2012, I decided we needed to take some further action since his issues were mounting, and it seemed he may have a severe rather than mild form of this disease. I started searching around some children’s hospital websites located near our area. The closest sickle cell specialists were in Washington State and Colorado. I found the name of a social worker who worked with the Children’s Hospital of Colorado located in Aurora, CO. My oldest brother and his family still had a home in Colorado Springs, so I thought it would be a good choice in case it would help to have some family nearby especially if multiple trips to Colorado would be required. We made an appointment to be seen by a hematologist at Children’s Hospital of Colorado in October of 2012, when Trayson was two months from being four years old. We would also have the noteworthy Transcranial Doppler (TCD) we had been informed about earlier on in his plan of care.
Our initial visit to the hospital in CO yielded a wealth of information and more specific information to Trayson’s version of the disease. They were impressed with how big and healthy he was for having SCD. Often times, kids with SCD appear to be small and sometimes frail. The examination and consultation with the hematologist was extremely informative and alarming at the same time. We were unaware of some things we really needed to pay more attention to such as the amount of water and calories needed each day for kids with SCD. There were many other things we didn’t know such as not using ice packs, trouble with temperature extremes, swimming issues, contact with reptiles, and cold weather problems. We could think back to some of our previous episodes and attribute them to these new and very specific things we were learning for the first time. It was surprising to learn that Trayson’s water requirement is 64 ounces a day, and he needs twice as many food calories as a normal child. The doctors assured us we were doing “something” right because other than the SCD, he seemed very healthy. They have even described him as one of the healthier looking kids they had seen living with SCD. At this visit, we were able to have his blood hyper-matched so that future blood transfusions would be better matched to Trayson’s blood since he has to have repeated transfusions. After several blood transfusions, your body starts to build up antigens, and the hyper-matching would avoid this as much as possible. We did receive some discouraging news from this initial visit. The Transcranial Doppler, the brain scan measuring velocity of blood flow to the brain, resulted in a “high-conditional” reading on one side which meant he had a high risk for stroke. This news was difficult to swallow because we had such positive thoughts regarding the brain scan. It was disappointing news but required immediate attention with no time to dwell. At this point for medications, Tray had been consistently on Penicillin as a preventative measure along with the different types of pain medication we had to try during each pain crisis. With the new findings, we would now add an additional medication called Hydroxyurea, a type of chemotherapy that would increase the amount of fetal hemoglobin. This medication would support the blood flow in his body because there would be less of the SS hemoglobin. Hemoglobin is a protein in the red blood cell that carries oxygen. Low hemoglobin is common and a major factor in SCD. The new medication was supposed to help with the stroke risk as well as decrease the number of pain episodes, instances of hospitalizations, and decrease the chance of Acute Chest Syndrome (a possibly fatal respiratory illness in SCD). Hydroxyurea is also said to raise his hemoglobin up at least 1.0. Low hemoglobin contributes to the fatigue and low oxygen saturation. We came away from our first consult with a blood specialist knowing a whole lot more, paying attention to every little detail, hyper-matched blood typing, and a new medication to add to the medical management of SCD. We were due to see our Colorado doctor and have a repeat TCD in six months to see if there was going to be any improvement in blood flow to the brain. We were scheduled to return to Children’s Hospital of CO in March of 2013.
After we returned home from our first Colorado medical visit, we came home to various pain episodes as well as entered respiratory season which always seemed to affect Trayson. In early January 2013, shortly after the New Year, Trayson fell ill while at Gramma’s house. I was at work, and Eric was working out of town. Tray’s temperature spiked to over 103 degrees, and we were definitely headed to the clinic while calling his pediatrician and knew we would most likely be admitted to the hospital until they could determine what was causing the high fever. We spent about four days in the local hospital, and Trayson was not getting better. He was deteriorating when we thought he should be getting better. The local doctors thought it would be best to consult with Children’s Hospital of CO. The Great Falls and Colorado doctors together decided after the usual tests, labs, and chest x-rays, he had developed Acute Chest Syndrome (ACS) and would need to be airlifted to Colorado to better deal with the disease. ACS can be fatal if not treated quickly. The news of the airlifting was especially devastating because Eric had not made it home from working out of town in Miles City, and we would fly before he could get back to us to say goodbye. Trayson, of course, was scared and wanted his daddy there by his side. It would be the next day before Daddy could finally be with us. While in the hospital in Colorado, we learned more about ACS and endured many, many bonks with Trayson including another blood transfusion. It took seven “roller coaster” days at Children’s Hospital Colorado for Trayson to be able to come back home to Great Falls. Our total hospital stay in January of 2013 was 11 days. Due to the recent blood transfusion, we had to push back our next TCD appointment another three months in order to get a proper reading. In March of 2013, we were back in the hospital in Great Falls needing another transfusion. This caused the TCD to be pushed into the summer time, most likely in July. Our July 2013 visit to Colorado yielded a great result from the TCD. It seemed the Hydroxyurea had helped with the velocity of blood flow to his brain, and it was now in acceptable levels for SCD. This was great news for us and relieved all of the family, just a little. We did not let our guard down though and stayed vigilant in Trayson’s care. We would be making trips to Colorado every three months now to see Tray’s doctors there. The fall of 2013 seemed to go pretty smoothly as long as we were staying focused and following doctor’s orders with hydration, calories, rest, medications, regular checkups and blood counts. In October of 2013, we were linked in with a new pediatric hematologist closer to our home but still located 3 ½ hours away in Billings, MT. We were able to see her every six months as well, so we could limit our trips to Colorado to every six months. This way Trayson could be seen by specialists consistently every three months. While seeing our hematologist in Billings, we were able to connect with a pediatric pulmonologist (lung doctor) as well.
Although the fall was a pretty healthy time, Trayson fell ill on Christmas Day of 2013. He had a high fever, and we took him to the ER to go through the gamut of x-rays, tests, blood counts, and IV antibiotics or antibiotic shots in the thighs. We were admitted just for an overnight stay (which was rare) and sent home after tests showed he had Para Influenza II. We kept him very secluded and rested over the next few days and thought we had him better. It was New Year’s Eve of 2013, and we had canceled our company for New Year’s due to what we deemed a setback in Tray’s health. He just didn’t seem quite right. After years of dealing with these issues, our instincts kicked in, and we knew something was wrong. We took him to the ER and ended up with an admission to the hospital for Para Influenza again. This hospital stay did not go as well. Trayson deteriorated quickly (common for SCD), and his Para Influenza turned into another bout with ACS. After two days in the local hospital, they were planning to airlift us to Colorado for our second January in a row. Once we made the decision to fly, it took several more hours before takeoff due to weather and night flying. We arrived in Colorado in the wee hours of the morning. When we arrived, Trayson had deteriorated so much that he needed to be moved to Pediatric Intensive Care (PICU) immediately and put on a Bi-Pap machine to help him breathe. When we left Great Falls, he was requiring two liters of oxygen, but when we arrived, he was up to five liters of oxygen and struggling to breathe. The doctors asked me how long he had been that way, but it had only been a few hours since we left Great Falls. He had just gone downhill so fast, and it was frightening. We spent a few days in PICU on Bi-Pap and were able to move up to the hematology floor. He seemed to be getting better each day and of course this is why they released us from PICU. The next night after being moved from PICU, Trayson had a fit of coughing. He couldn’t stop coughing which caused him to cry. This coughing and crying was heartbreaking because we could not do anything to console him. As a parent, all we wanted was to take his pain away. The coughing and crying continued through all of our comforting, and this alerted our nurse. She came in to see what was going on and listen to his lungs but found him to be struggling to breathe. Then, suddenly, Trayson stopped breathing while Eric and I helplessly looked on. The nurse was quick to react and had a Code Blue going within seconds. Teams of doctors and nurses came in with some working on Trayson and others trying to console us. From my perspective, I could only stare at Trayson and will him to fight through this and come back to us. Trayson is such a fighter. He was able to regain his breathing again. We were immediately transferred back to PICU to go back on Bi-Pap until we figured out what was going on. Trayson was able to tell me later that day that he was having pain in his chest and abdomen which no one including doctors knew about. Trayson said he thought if he said he wasn’t having any pain, he would get to go back home. The pain he was having was causing him to take short, shallow breaths rather than the deep breaths required to clear his lungs. We immediately started him on round the clock morphine to alleviate this pain so he could breathe correctly to start healing. After two days in the PICU again, we were moved back to the hematology floor where we stayed for several more days to make sure he was out of the woods. Total hospital stay between Great Falls and Colorado was 14 days this time with most of it at Children’s of CO. After returning home, we felt like we had been in some crazy nightmare, but we learned a lot about Trayson, the patient. We began taking abdominal pain and chest pain even more seriously since they affected his breathing so much this go round. We were also able to get a pain medication, Dilaudid, which actually works for his severe pain. We keep this medication filled all the time in case we need something strong to battle the pain. Now, Trayson is very good about declaring pain and able to put it on a pain scale of 1-10. He knows anything above a five will need Ibuprofen and possibly Dilaudid. If he rates pain at seven or higher, we will treat with Dilaudid first thing to stay on top of the pain so it doesn’t affect his breathing. His arms and legs suffer pain as well, but these areas don’t affect the way he breathes as much and are easier to manage from home with pain meds. After this second airlifting, we continued with our follow up appointments to Billings later on in January 2014. We were scheduled to be back in Colorado for appointments the following April.
Before April came, Trayson was admitted to the hospital in March of 2014 for a respiratory illness. They found some infiltrates on his chest x-ray. This would be his 3rd bout with ACS although this occurrence didn’t require airlifting to Denver. We were able to get through the crisis here in Great Falls but knowing we would be in for some tough decision-making going forward. SCD has always required a lot of decision-making. I just knew we were on the brink of more decisions regarding Tray’s life. Three bouts of ACS by age five are quite a few for SCD and can cause lung damage as well as death. As we had seen, it causes the body to deteriorate quickly from bad to worse in very short intervals of time. We were currently looking at the possibility of lung damage.
At our April 2014 appointment in Colorado, we and the doctors decided to explore the option of a bone marrow transplant (BMT). The first step in exploring BMT is to swab all three of us to see if Eric and I happen to match. Then, the search for DNA matches for Trayson began. The doctors told us it would take about six weeks to find out if he has a match out there. My hopes were very high at first, but then I started looking into the matching process. My hopes began to diminish because it seemed so out of reach to have unrelated matched DNA. In late May of 2014, we were informed that Trayson actually has thousands of matches out there. These are gold standard 10 of 10 matches, and he has lots of gold standard cord blood matches as well. This was fantastic news for us. We were excited to explore the option of BMT!
In June of 2014, we were informed that Trayson would be nominated for a Make a Wish Foundation wish. Anything he would like to wish for could possibly be granted if he was selected. We did receive word about mid-summer that Trayson was actually selected, and the process would be started to grant his wish. His wish…he wants to meet Mickey Mouse and Darth Vader!!! Perfect! His wish is due to come true on May 26, 2015!!! Our local high school, Great Falls High School Bison, was able to sponsor Trayson for the whole wish! Great Falls High School has been very kind to us and supported Trayson in countless ways through fundraising and raising awareness about SCD. We are forever indebted to the students, staff, and administration at GFHS.
We all knew July of 2014 was going to be a busy month for Trayson. He even knew he would be busy traveling to both Billings and Colorado and could tell everyone how many days he would stay in a motel (loves motels!). In the middle of July, we were heading to Billings to have a sleep study along with our regular visit to our two specialists there. The pulmonologist ordered the sleep study which measures almost everything under the sun it seems. Trayson was quite a trooper with about 50 wires coming out of him! We later were informed of the sleep study results, and once again, there was good news and bad news. The good news was great news, but the bad news certainly overshadowed anything else. They discovered his oxygen saturation to dip into the 80s for 72% of the night. His average oxygen saturation over the 7.5 hours of sleep was 88%. This would not be positive news for his young organs. This is information I wished I had received earlier. These results would yield more medical management from home. Trayson would have to begin sleeping with oxygen every night. We would start immediately at ½ a liter and see how it goes. Eventually, we did move down to a ¼ liter, but Trayson does not enjoy sleeping with oxygen every night. He often asks how long he will have to wear the oxygen. It is a very hard question to answer. In addition to the oxygen at night, the pulmonologist recommended we start on an asthma regiment recommended by colleagues in Georgia. Tray was to begin taking another oral medication in addition to an inhaler twice a day. Since August of 2014, Trayson takes an inhaler, one pill and a vitamin in the morning, and he takes four pills and the inhaler in the evening along with the required oxygen at night. It seems like a lot of medication for a now six year old, but this is how we are supposed to medically manage SCD.
We would piggy back the July 2014 Billings appointment with another trip to Colorado for a Bone Marrow Transplant consult with an assigned transplant doctor at Children’s. Since we were fortunate to have some quality bone marrow matches for Trayson, we just had to explore our options. Knowledge is power. There we sat; the three of us, going through an exam of Tray and listening to a doctor explain BMT to us. Trayson was in the room, but he was busy playing so paid no attention to what we were doing. My sister-in-law, Kristen, was nice enough to videoconference into the consult, so we could have an extra set of ears and questions. The pros and cons of BMT are aplenty and were explained in great detail. We filtered through the science of it all and were left feeling extremely overwhelmed by the whole experience. It is hard to put into words, but I will try. Trayson has a very severe case of Sickle Cell Disease. The only known cure for this disease is bone marrow transplant. There are no guarantees. There will be complications. He will have chemotherapy for 7-10 days to wipe out all of his bone marrow including his immune system. Chemotherapy will be very difficult, and he will be very sick. He will lose his hair and have various side effects ranging from mild to severe. There is a high risk of graft vs. host disease (GVHD) where his body fights back against the new marrow. He will be hospitalized for anywhere from 4-6 months and will not be able to go back to school for a year. The ultimate risk is death. These words haunt me to this day. These are the words that create fear for this decision; however, BMT is the only known cure for SCD. Needless to say, we left the consult full of tough emotions and tough decisions. Trayson left the consult and couldn’t wait to get back to the motel (loves motels!). He was oblivious to the current news, and we let him be for now. Eric and I decided to make the rest of the Colorado trip enjoyable for Trayson and keep our emotions at bay until we returned home.
After returning home, my sister–in-law that was listening in to our consult invited us to come to North Carolina for a visit to the BMT doctors in their area. We were lucky to have this opportunity for a second opinion regarding BMT. In August of 2014, Tray and I flew to North Carolina to consult with doctors there. This visit was eerily similar to the first consult, meaning the second opinion was the same as the first. The only difference…I had to process this time without Eric since he stayed back in Great Falls to work. I felt as if this consult was a good confirmation of what may need to happen for Trayson’s sake.
At this point, returning from North Carolina, Eric and I really needed to sit down and talk about the decision facing us…whether or not to go forward with the BMT. This is the point in time we began the new medications to try to ward off any respiratory illnesses before they hit to avoid another ACS. It seemed a lot had transpired in the summer of 2014 where Trayson’s health was concerned. Shortly after returning from NC, Kristen set up a phone conference with a doctor in Cincinnati who was kind enough to chat with me about Hydroxyurea. This doctor is an expert on this drug we had been giving Trayson since 2012, but more noteworthy, he is not a transplant doctor. It was nice to hear the “other side” of the story from a doctor who believed in the medical management and living with SCD. He made a lot of sense to me and also asked me if we had “tried everything” before deciding to go to transplant. After discussing this information with Eric, we felt like we needed to give the new oxygen treatment and asthma medications an honest chance.
Trayson was due to start kindergarten at Lincoln Elementary, where I also teach, in September of 2014. He was indifferent about starting kindergarten, but after meeting his teacher, he felt a lot better about beginning the school year. School would be challenging in Montana due to the weather extremes, mostly cold weather issues which would most likely affect Trayson socially due to not being able to participate in outdoor activities such as recess. He is required to stay inside if the temperature dips below 50 degrees, if it is snowing, or there are extremely windy conditions. There are several other issues with SCD that could impact his schooling as well, so we immediately put an educational plan, a 504, in place to make sure he would get the services he needs academically in case of any complications that could arise. We already knew there would be several absences over the course of the year because of the various illnesses. We made sure the Lincoln staff was informed of his unique situation. The staff at Lincoln has been accommodating Trayson every step of the way. They have always been a huge support to our family, including emotional, physical, and financial support. We couldn’t have asked for a better situation for Trayson’s educational experience. He quickly made lots of new and fantastic friends. School really opened his eyes to the differences among him and his classmates. Starting school made Trayson realize how different he is from other kids, and how much he wants to be a normal child like his friends in class. Despite being around lots of other kids at school, he seemed to be staying pretty healthy through the fall of 2014. This was quite promising to us, and we attributed the good health to the addition of oxygen at night and the new asthma medications we were trying. We were hopeful that things would continue on smoothly from here.
In October of 2014, we traveled to Billings for our regular appointments and informed our hematologist that we would be “tabling” our discussion regarding transplant for now and would see how Tray does through the winter months and respiratory season with these new things we were trying. The conversation with both the hematologist and pulmonologist went very well, and they were supportive of our thinking at the time. From our perspective, we were having a hard time taking our seemingly healthy little boy and making him very sick and possibly ending in death. To us, the risk outweighed the reward at this point. These things haunted us, plus with these new medications and oxygen, it only seemed right to try everything possible before making a decision that could potentially end our son’s life. The decision was officially made, and a weight was lifted off of us. Now, we will do our best to keep Trayson healthy through the dreaded month of January and the rest of the respiratory season.
Unfortunately, when we returned home from Billings in October of 2014, Trayson fell ill. This illness caused Tray to miss out on trick or treating on Halloween, but a few nice friends of ours allowed us to “make up” Halloween the following weekend. We were not hospitalized, but this illness did cause his hemoglobin to drop below 7.0 and required a transfusion along with several missed school days. He bounced back from this illness after having the transfusion, resting up, and supplementing with oxygen at home to keep him above 95%. His health improved, and he was back into the swing of things at school.
Trayson turned six years old on Dec. 9, 2014, and he seemed to be doing very well after the setback in October. He was looking forward to Christmas, but we as parents, were not without worry. This is the time of year Trayson struggles the most with his health. When we had a two week break from school, we kept him in a “bubble” at home all but about two days. We felt we could protect him from the illnesses that were out there during this rough time of year. We were successful in keeping him healthy through December and most of January and were very excited at the possibility of staying relatively healthy throughout respiratory season.
In the latter part of January 2015, Tray did fall ill with a high fever which was treated by the clinic with strong antibiotics and sent home to manage with oxygen, rest, and medicine. We were happy to be able to manage this illness at home which seemed easier with oxygen at our fingertips. When February came around, we felt as if he was better but decided to hold him out from school an extra day and the weekend. By then, he surely would be well enough to go back to school. During this illness, we were having his blood counts checked often to make sure his hemoglobin stayed above 7.0 as well as a chest x-ray to make sure his lungs were staying clear. After the weekend, Eric took him in for blood counts, and his hemoglobin had dropped a bit. We were scheduled to have a blood transfusion after this drop in hemoglobin, but he wasn’t having too many symptoms of illness. The next day, he woke up coughing on the day of the scheduled transfusion. The pediatrician suggested another chest x-ray before the transfusion, and our routine blood transfusion to boost hemoglobin turned into a full blown hospitalization. The chest x-ray showed infiltrates in his right lung that were not there two days prior. The blood transfusion went fine, but our worries shifted to Trayson’s next bout with ACS. This would be his fourth instance of Acute Chest Syndrome. This time his fever spiked, and he went from seeming fine to being very, very ill. This one came on very suddenly and didn’t waste any time. Colorado doctors consulted with our doctors here and decided immediately to airlift to Children’s Hospital for our third time. This was a confusing time for Trayson because he even recognized himself getting better and then suddenly worse. We arrived in Colorado to the teams of doctors and nurses we had come to know over the last few years. This time, we made it before Trayson was in dire need. Quick decision-making and experience with SCD and ACS made this hospital stay shorter, but this visit was an eye opener for both Eric and me. We spent seven days in the hospital and were reintroduced to the BMT doctor and had a very candid conversation about Trayson and his future with SCD. We returned from Colorado knowing the conversation about BMT was back on the table, and now our decision time was limited. We would need to let the BMT team know our decision by the end of February 2015 to have enough time to find a donor, harvest marrow, and be ready for a summer transplant.
Eric and I spent a great deal of time weighing our options. It was clear that medical management of SCD may not be working for our son. At any point, on any day, Trayson could be taken from us because of this disease. It is a very real experience. At the end of February 2015, I made the call to the BMT team at Children’s Hospital of Colorado to set up his first appointment on June 16, 2015. We all will be in the fight of our lives to save Trayson’s life. We will never feel comfortable, but we feel confident we have made the right decision for Trayson.
For the time being, Trayson is receiving chronic blood transfusions every other week to keep him as healthy as possible leading up to transplant. These blood transfusions are a huge time commitment, but Trayson is adapting as well as he always does to adversity.
Every day, Trayson fights an internal battle we know nothing about. Sickle Cell Disease is a horrific battle and often results in short life expectancy or poor quality of life. Everyone living with the disease goes through different experiences and complications. Trayson is our hero, and we love him more than anything in the world. He is nothing less than a SICKLE CELL WARRIOR, and WE WILL FIGHT this battle together no matter what.
Organiser
Trayson Harrell
Organiser
Great Falls, MT


